The smart Trick of How To Write A Proposal To Pain Management Clinic For Additiction Prevention Services That Nobody is Talking About
Given that lots of kinds of chronic discomfort may need a complex treatment plan along with specialized interventional techniques, pain specialists today should have more training than in the past, and you need to find out about how your discomfort doctor was trained and whether she or he has board accreditation in discomfort management.
The majority of fellowship programs are related to anesthesiology residency training programs. There are likewise fellowship programs associated with neurology and physical medicine and rehab residency programs. The fellowship consists of a minimum of one year of training in all elements of pain management after conclusion residency training. When a physician has actually become board certified in their primary specialty and has actually finished an accredited fellowship, they become qualified for subspecialty board accreditation in discomfort management by the American Board of Anesthesiology, The American Board of Psychiatry and The American Board of Neurology, or the American Board of Physical Medicine and Rehab.
In addition to learning about your discomfort doctors training and board certification, you likewise need to ask whether they have experience with your specific pain condition and what kinds of treatments they use. Do they only carry out treatments or do they use a multidisciplinary approach to pain management? Who do they refer to for other treatment choices such as surgical treatment, mental assistance or alternative treatments? How http://travisyadd232.bearsfanteamshop.com/what-does-what-to-expect-when-you-go-to-a-pain-clinic-mean can they be reached if concerns or issues emerge? What is their overall approach of discomfort management? The best method to be referred to a pain management specialist is through your primary care doctor.
Clients are also frequently referred by professionals who deal with different kinds of discomfort issues. Back cosmetic surgeons, neurologists, cancer medical professionals, along with other experts generally work routinely with a pain physician and can refer you to one. On your very first visit to a discomfort management professional, she or he will be familiar with you and begin to examine your specific discomfort problem.
The questions you are asked and the health examination will focus on your particular problem, but your pain doctor will want to know about past and existing medical history too. Often you will be provided a questionnaire prior to your very first go to that will ask comprehensive questions about your pain issue, and you will probably be asked to bring any imaging research studies (such as X-rays, calculated tomography [CAT] scans, or magnetic resonance imaging [MRI] scans) or other tests that have currently been done.
If so, you might need a motorist to take you home. Most importantly, this check out is an opportunity for your pain physician to begin to analyze all of this new details and talk about with you a preliminary evaluation of your pain problem. He or she might know exactly what is triggering your discomfort, or maybe additional diagnostic procedures will be required.
A pain center is a healthcare resource that focuses on the medical diagnosis, management and treatment of chronic discomfort. Within many clinics, experts that concentrate on different discomfort types and conditions are offered. A discomfort management expert is a physician with additional training in the medical diagnosis and treatment of pain.
What Does Clinic How To Tell If Someone Is In Pain Or Trying To Get Pain click here Meds Do?

Pain management specialists prescribe medications, perform treatments (such as back injections and nerve blocks) and suggest therapies to treat pain. The very first check out to a discomfort management clinic normally involves a consultation with a general practitioner, internist, nurse professional or medical assistant. The visit usually involves an in-depth examination of the individual's discomfort history, a physical examination, pain assessment, and diagnostic tests.
Depending upon the origin and severity of chronic discomfort, an appointment for an assessment with a various discomfort expert within the center might be suggested. Physicians normally available at a pain clinic consist of the following: General PractitionersInternists NeurologistsRheumatologistsAnesthesiologistsOrthopedistsPhysiatristsPsychiatristsOther specialists at a discomfort center may consist of physiotherapists, occupational therapists, chiropractic specialists, acupuncturists and psychologists.
A discomfort management professional is a medical professional who assesses your discomfort and treats a wide variety of discomfort issues. A pain management medical professional deals with abrupt pain problems such as headaches and numerous types of lasting, chronic, discomfort such as low pain in the back. Clients are seen in a discomfort clinic and can go home the very same day.
The types of pain dealt with by a pain management doctor fall under 3 main groups. The very first is pain due to direct tissue injury, such as arthritis. The 2nd type of discomfort is due to nerve injury or a nerve system disease, such as a stroke. The third type of pain is a mix of tissue and nerve injury, such as back discomfort. what is pain management clinic.

First, they gain a broad education in medical school. Then, they get another four years of hands-on training in a field like anesthesiology, physical medicine and rehabilitation, or neurology. Finally, they complete another year of training, that focuses exclusively on treating pain. This causes a certificate from the American Board of Discomfort Medication.
Nevertheless, for advanced pain treatment, you will be sent out to a pain management physician. Discomfort management physicians are trained to treat you in a step-wise way. First line treatment involves medications (anti-inflammatories, muscle relaxants, anti-depressants) and injections that numb pain (nerve blocks or back injections). TENS (Transcutaneous electrical nerve stimulators systems that utilize skin pads to deliver low-voltage electrical current to painful locations) might also be utilized.
Throughout RFA, heat or chemical agents are used to a nerve in order to stop discomfort signals. It is used for persistent discomfort issues such as arthritis of the spine. Viscosupplementation is the injection of lubricating fluid into joints, used for arthritis discomfort. At this stage, the medical professional may likewise prescribe more powerful medications.
Things about How Many Hydrocodones Do I Need To Take To Show Up On A Urine Test At A Pain Clinic
These treatments act to relieve pain at the level of the spine cable, which is the body's nerve center for picking up pain. Regenerative (stem cell) treatment is another choice at this stageFor more information on treatments provided by pain management physicians, click here.Communication lies at the heart of a great doctor-patient relationship.
Preferable qualities in a discomfort doctor/pain center: Extensive understanding of discomfort disordersAbility to assess patients with difficult pain disordersAppropriate prescribing of medications for pain problemsAn ability to utilize different diagnostic tests to identify the cause of painSkill with treatments (nerve blocks, spinal injections, pain pumps) A great network of outside service Drug and Alcohol Treatment Center providers where the patient can be sent for physical therapy, psychological assistance or surgical evaluationTreatment that is in line with a client's desires and belief systemUp-to-date equipmentHelpful office staffPain patients are seen in an outpatient pain center that has procedure rooms, with ultrasound and X-ray imaging (what medication in clinic abdominal pain).
Some discomfort medical professionals may use you sedation throughout the treatments. However, this is not required oftentimes. In a hospital, "Twilight" anesthesia might be provided to a patient, as required. On the very first go to, a discomfort management physician will ask you questions about your pain symptoms. She or he may likewise take a look at your past records, your medication list, and prior diagnostic research studies (X-ray, MRI, CT).
Indicators on When Is Comprehensive Pain Clinic Opening Back Up You Should Know
Considering that many kinds of chronic pain might require a complex treatment plan as well as specialized interventional strategies, discomfort specialists today must have more training than in the past, and you must discover how your pain doctor was trained and whether he or she has board certification in discomfort management.
A lot of fellowship programs are connected with anesthesiology residency training programs. There are also fellowship programs related to neurology and physical medicine and rehab residency programs. The fellowship consists of a minimum of one year of training in all aspects of pain management after conclusion residency training. When a physician has actually become board accredited in their primary specialty and has finished a certified fellowship, they become qualified for subspecialty board accreditation in pain management by the American Board of Anesthesiology, The American Board of Psychiatry and The American Board of Neurology, or the American Board of Physical Medication and Rehab.
In addition to learning more about your pain physicians training and board accreditation, you likewise ought to ask whether they have experience with your particular pain condition and what kinds of treatments they use. Do they just perform procedures or do they use a multidisciplinary approach to discomfort management? Who do they refer to for other treatment options such as surgical treatment, psychological assistance or alternative treatments? How can they be reached if concerns or issues occur? What is their general viewpoint of pain management? The very best method to be referred to a pain management expert is through your medical care doctor.
Clients are also typically referred by specialists who handle various types of discomfort problems. Back cosmetic surgeons, neurologists, cancer doctors, as well as other professionals usually work routinely with a discomfort doctor and can refer you to one. On your very first visit to a discomfort management expert, he or she will be familiar with you and start to evaluate your specific discomfort problem.
The concerns you are asked and the physical evaluation will focus on your specific issue, however your discomfort physician will wish to know about previous and current case history as well. Often you will be given a survey before your first check out that will ask in-depth concerns about your pain problem, and you will most likely be asked to bring any imaging research studies (such as X-rays, computed tomography [CAT] scans, or magnetic resonance imaging [MRI] scans) or other tests that have actually already been done.
If so, you may require a chauffeur to take you home. Most importantly, this see is a chance for your discomfort physician http://travisyadd232.bearsfanteamshop.com/what-does-what-to-expect-when-you-go-to-a-pain-clinic-mean to begin to analyze all of this brand-new information and discuss with you a preliminary assessment of your pain issue. He or she might understand exactly what is triggering your pain, or maybe further diagnostic procedures will be needed.
A discomfort clinic is a healthcare resource that focuses on the medical diagnosis, management and treatment of persistent pain. Within numerous centers, specialists that focus on different pain types and conditions are available. A pain management expert is a doctor with extra training in the diagnosis and treatment of discomfort.
How What Does A Pain Clinic Drug Test Test For can Drug and Alcohol Treatment Center Save You Time, Stress, and Money.
Pain management professionals recommend medications, perform treatments (such as spine injections and nerve blocks) and suggest therapies to treat discomfort. The first check out to a discomfort management center generally involves a visit with a family doctor, internist, nurse practitioner or medical assistant. The see usually involves an in-depth examination of the individual's discomfort history, a physical examination, discomfort assessment, and diagnostic tests.
Depending on the origin and intensity of persistent pain, a visit for an assessment with a different pain professional within the center might be suggested. Physicians usually available at a pain center consist of the following: General PractitionersInternists NeurologistsRheumatologistsAnesthesiologistsOrthopedistsPhysiatristsPsychiatristsOther experts at a discomfort center may include physiotherapists, occupational therapists, chiropractic doctors, acupuncturists and psychologists.
A discomfort management expert is a physician who evaluates your discomfort and deals with a broad variety of pain issues. A discomfort management medical professional deals with abrupt discomfort issues such as headaches and lots of kinds of lasting, chronic, pain such as low neck and back pain. Clients are seen in a discomfort clinic and can go home the very same day.
The types of discomfort treated by a discomfort management physician fall under 3 main groups. The very first is discomfort due to direct tissue injury, such as arthritis. The second type of pain is because of nerve injury or a worried system disease, such as a stroke. The 3rd kind of discomfort is a mix of tissue and nerve injury, such as pain in the back. how pelvic pain exam done in minute clinic.
First, they gain a broad education in medical school. Then, they get another four years of hands-on training in a field like anesthesiology, physical medicine and rehabilitation, or neurology. Finally, they complete another year of training, that focuses solely on treating discomfort. This results in a certificate from the American Board of Pain Medicine.

Nevertheless, for innovative discomfort treatment, you will be sent to a discomfort management physician. Pain management medical professionals are trained to treat you in a step-wise way. Very first line treatment involves medications (anti-inflammatories, muscle relaxants, anti-depressants) and injections that numb pain (nerve obstructs or spinal injections). TENS (Transcutaneous electrical nerve stimulators units that utilize skin pads to deliver low-voltage electrical existing to uncomfortable areas) might likewise be utilized.

Throughout RFA, heat or chemical representatives are applied to a nerve in order to stop discomfort signals. It is utilized for persistent pain issues such as arthritis of the spine. Viscosupplementation is the injection of lubricating fluid into joints, utilized for arthritis pain. At this phase, the doctor might also recommend more powerful medications.
Top Guidelines Of What Is The Doctor's Name At Eureka Pain Clinic
These treatments act to ease discomfort at the level of the spine, which is the body's nerve center for sensing pain. Regenerative (stem cell) treatment is another alternative at this stageFor more info on treatments used by pain management physicians, click here.Communication lies at the heart of an excellent doctor-patient relationship.
Preferable qualities in a discomfort doctor/pain clinic: Thorough understanding of discomfort disordersAbility to examine clients with difficult discomfort disordersAppropriate prescribing of medications for discomfort problemsAn capability to use different diagnostic tests to identify the cause of painSkill with procedures (nerve blocks, spine injections, discomfort pumps) An excellent network of outdoors suppliers where the patient can be sent for physical therapy, mental assistance or surgical evaluationTreatment that remains in line with a client's wishes and belief systemUp-to-date equipmentHelpful workplace staffPain patients are seen in an outpatient discomfort center that has treatment click here rooms, with ultrasound and X-ray imaging (who to complain to about pain clinic).
Some pain physicians may use you sedation during the treatments. However, this is not required in a lot of cases. In a health center, "Golden" anesthesia may be given to a client, as needed. On the very first visit, a discomfort management doctor will ask you questions about your discomfort signs. He or she may likewise look at your past records, your medication list, and prior diagnostic studies (X-ray, MRI, CT).
10 Easy Facts About How Many Patients Can A Pain Clinic Have Described
Since many kinds of chronic discomfort might need a complex treatment strategy as well as specialized interventional techniques, discomfort specialists today should have more training than in the past, and you must discover how your pain physician was trained and whether she or he has board accreditation in pain management.
A lot of fellowship programs are associated with anesthesiology residency training programs. There are likewise fellowship programs connected with neurology and physical medication and rehab residency programs. The fellowship consists of a minimum of one year of training in all elements of discomfort management after completion residency training. When a doctor has ended up being board certified in their main specialty and has actually completed an accredited fellowship, they end up being qualified for subspecialty board certification in pain management by the American Board of Anesthesiology, The American Board of Psychiatry and The American Board of Neurology, or the American Board of Physical Medicine and Rehabilitation.
In addition to discovering your pain physicians training and board certification, you also should ask whether they have experience with your particular discomfort condition and what types of treatments they use. Do they only carry out procedures or do they utilize a multidisciplinary technique to pain management? Who do they describe for other treatment choices such as surgical treatment, psychological assistance or alternative therapies? How can they be reached if concerns or issues develop? What is their total viewpoint of pain management? The very best way to be referred to a discomfort management expert is through your medical care physician.
Patients are likewise typically referred by professionals who deal with different kinds of discomfort problems. Back surgeons, neurologists, cancer physicians, as well as other experts normally work frequently with a discomfort doctor and can refer you to one. On your first check out to a pain management expert, she or he will learn more about you and begin to examine your particular discomfort problem.
The concerns you are asked and the physical evaluation will focus on your specific problem, however your discomfort physician will need to know about past and present case history as well. Often you will be provided a survey prior to your first visit that will ask in-depth questions about your pain problem, and you will most likely be asked to bring any imaging research studies (such as X-rays, computed tomography [CAT] scans, or magnetic resonance imaging [MRI] Drug and Alcohol Treatment Center scans) or other tests that have currently been done.
If so, you may require a driver to take you home. Most importantly, this see is an opportunity for your pain doctor to begin to evaluate all of this brand-new info and talk about with you an initial assessment of your discomfort problem. He or she may understand exactly what is triggering your discomfort, or possibly further diagnostic treatments will be required.

A discomfort center is a health care resource that concentrates on the diagnosis, management and treatment of chronic pain. Within many clinics, specialists that focus on various discomfort types and conditions are readily available. A pain management expert is a doctor with additional training in the medical diagnosis and treatment of discomfort.
How How Long Does Oxyconton Stay In Your System For A Pain Clinic Urine Test can Save You Time, Stress, and Money.

Pain management professionals prescribe medications, carry out treatments (such as spine injections and nerve blocks) and suggest therapies to treat pain. The very first visit to a pain management center normally includes a visit with a family doctor, internist, nurse practitioner or medical assistant. The visit generally involves a detailed examination of the individual's pain history, a physical test, pain evaluation, and diagnostic tests.
Depending upon the origin and severity of chronic pain, a visit for a consultation with a various pain professional within the clinic might be recommended. Physicians generally readily available at a pain clinic consist of the following: General PractitionersInternists NeurologistsRheumatologistsAnesthesiologistsOrthopedistsPhysiatristsPsychiatristsOther specialists at a pain center might include physiotherapists, occupational therapists, chiropractic specialists, acupuncturists and psychologists.
A pain management expert is a medical professional who assesses your pain click here and treats a wide variety of pain issues. A discomfort management doctor treats sudden pain issues such as headaches and lots of kinds of long-lasting, persistent, pain such as low pain in the back. Clients are seen in a discomfort center and can go home the very same day.
The kinds of pain treated by a pain management doctor fall under 3 primary groups. The very first is discomfort due to direct tissue injury, such as arthritis. The 2nd type of discomfort is because of nerve injury or a nerve system disease, such as a stroke. The 3rd type of discomfort is a mix of tissue and nerve injury, such as neck and back pain. who are the names of pa's and np's at sanford pain clinic.
Initially, they gain a broad education in medical school. Then, they get another 4 years of hands-on training in a field like anesthesiology, physical medication and rehabilitation, or neurology. Finally, they complete another year of training, that focuses exclusively on treating pain. This leads to a certificate from the American Board of Pain Medicine.
Nevertheless, for innovative discomfort treatment, you will be sent to a pain management physician. Pain management doctors are trained to treat you in a step-wise way. Very first line treatment includes medications (anti-inflammatories, muscle relaxants, anti-depressants) and injections that numb pain (nerve blocks or back injections). 10S (Transcutaneous electrical nerve stimulators systems that use skin pads to deliver low-voltage electrical existing to painful areas) might also be used.
Throughout RFA, heat or chemical representatives are applied to a nerve in order to stop discomfort signals. It is utilized for chronic pain problems such as arthritis of the spine. Viscosupplementation is the injection of lubricating fluid into joints, utilized for arthritis discomfort. At this stage, the doctor might also recommend stronger medications.
The Only Guide to How Long Do You Need To Be Off Antibiotics Before Pain Clinic Shots
These treatments act to eliminate pain at the level of the spine cable, which is the body's control center for sensing discomfort. Regenerative (stem cell) treatment is another choice at this stageFor more info on treatments provided by pain management physicians, click here.Communication lies at the heart of a good doctor-patient relationship.
Desirable qualities in a discomfort doctor/pain clinic: Extensive understanding of pain disordersAbility to assess patients with hard pain disordersAppropriate prescribing of medications for pain problemsAn ability to utilize various diagnostic tests to determine the reason for painSkill with procedures (nerve blocks, spinal injections, discomfort pumps) An excellent network of outside companies where the client can be sent for physical therapy, psychological support or surgical evaluationTreatment that remains in line with a patient's desires and belief systemUp-to-date equipmentHelpful office staffPain clients are seen in an outpatient http://travisyadd232.bearsfanteamshop.com/what-does-what-to-expect-when-you-go-to-a-pain-clinic-mean pain clinic that has procedure rooms, with ultrasound and X-ray imaging (who are the names of pa's and np's at sanford pain clinic).
Some discomfort physicians might offer you sedation throughout the treatments. Nevertheless, this is not required in a lot of cases. In a healthcare facility, "Golden" anesthesia might be provided to a client, as needed. On the very first see, a discomfort management medical professional will ask you questions about your pain signs. She or he may also look at your past records, your medication list, and prior diagnostic studies (X-ray, MRI, CT).
See This Report about How Does A Pain Management Clinic Help People
Epidural injections Facet injections Radiofrequency ablation Intrathecal pumps Discography Vertebroplasty SI joint injection Spinal injections Spine stimulation Percutaneous discectomy Intradiscal treatments Stellate ganglion blockade. You may wonder what discomfort management physicians do that is various from your medical care physician, and the answer is a lot. The pain management field has actually grown over the years and continues to become a growing number of complex, making it that a lot more important to work with a professional.
While your medical care physician is experienced about a variety of health and physical concerns, they have actually not gotten the very same level of training on particular conditions that a professional has gotten. In truth, in 2011 just four medical schools in the entire United States included courses that focused exclusively on pain in as a part of required curriculum.
Part of what our pain management physicians do after medical school includes completing additional residencies, internships and fellowship training particular to the treatment of persistent discomfort. This extra training not only deepens their knowledge of persistent discomfort itself, however also the interventional procedures that can help in reducing suffering and increase quality of life.
Our method is to utilize the most ingenious and minimally invasive techniques the industry needs to offer. To arrange a consultation, find a place near you. what i need for open a pain clinic office in ms. Resources: Institute of Medicine (US) Committee on Advancing Pain Research Study, Care, and Education. Alleviating Discomfort in America: A Plan for Changing Prevention, Care, Education, and Research study.
Pain management doctors doctors who concentrate on the assessment, diagnosis, and treatment of pain have advanced training that qualifies them as your finest source of treatment if you are experiencing any type of discomfort due to disease or injury. After a general residency, these doctors go through an additional 1 year fellowship in discomfort management, and they are board-certified in a specialty, such as sport injuries or cancer pain.
How To Get Into A Pain Management Clinic for Beginners
Discomfort management doctors usually see clients with pain in the low back, knee, head, hip, and neck. Common conditions dealt with is these physicians consist of: arthritis, fibromyalgia, migraines, sciatica, and more. For something, they diagnose the specific cause of your discomfort and the underlying conditions that result in it.
It might be brought on by numerous conditions varying from poor posture at your work desk to a herniated disc to a degenerative condition like arthritis. When a discomfort management physician diagnoses your pain, he or she can find the therapy that works best for you based on their specialized training and the most recent research study.
Pain doctors frequently use a wide variety of nonsurgical, interventional treatments in addition to complementary treatments as a way of reducing the quantity of medication you require to take or to avoid the need for surgical treatment. These might consist of massage, a weight reduction routine, acupuncture, workout, yoga, meditation, physical treatment, dietary modifications, or chiropractic care.
Depending on the seriousness of your specific condition, they might also recommend epidural steroid injections, nerve blocks, joint injections, radiofrequency ablation, spine stimulation, or neuromodulation. If none of these approaches are reliable in reducing your pain, surgery may be an option of last option. In any case, your pain management medical professional will collaborate treatment between multiple doctors and health care professionals.
Because role, your pain management doctor serves as a supporter dedicated to alleviating your symptoms. For more information about how a discomfort management doctor can assist you conquer your pain problems, speak with the experts at Pain Specialists of Austin and Central Texas Discomfort Center. We assist patients like you every day.
The Of What Happens When You Are Referred To A Pain Clinic
My associate and I pulled into the collapsing parking lot. It was just 9:30 a.m., however the car park was nearly filled to capability with vehicles and people crushing about and walking in and out of the old structure, its signs hardly detectable. I had actually been kept to perform an assessment of another medical practice under federal investigation for releasing countless dosages of oxycodone "for other than a legitimate medical function." The entrance to the pharmacy on the first floor of the structure was manned by a guard, and neon-colored flyers cluttered the surrounding walls.

This was not a great impression. We awaited the elevator to the third flooring, in addition to a half-dozen individuals in their mid-20s, here early-30s. We stepped off the elevator and headed to Suite 322, and as anticipated, so did everyone else. Numerous individuals were seated on the flooring in the hallway outside the medical suite and an older woman in a wheelchair was parked against the wall.
In addition to the standard workplace waiting space chairs, a number of old folding chairs had also been generated. There were no magazines, no side tables, just a dusty flooring lamp and some random medical brochures inside a publication rack bolted to the wall. It was clear that everyone had lacked perseverance, individuals were grumbling and appeared to be contending for an award for who had actually been waiting the longest.
We stood in line at the reception counter behind a guy demanding to understand when 2 of his patients back there were going to be out. The receptionist had no response for him. The receptionist did not even take a look at me or my partner, she just handed me a brand-new patient intake form and informed me to have a seat.

I discovered that somebody had actually already pulled a couple dozen patient charts and established a card table in the examination room for us. The receptionist used us coffee and stated the physician would be in to consult with us as soon as she could. Right away, we saw the assessment room was barren.
How Many Oxycodone Pills Can You Be Short Pain Clinic Fundamentals Explained
We sat down and started to examine the patient charts while we awaited the chance to interview our customer relating to client care and practice policies. how to set up a pain management clinic. When the medical professional arrived for her interview, she began with her background and education-- she had just recently been hired to work locum tenens by the owner of the practice and had actually signed on for 6 months.
About How Long Do You Need To Be Off Antibiotics Before Pain Clinic Shots
Epidural injections Facet injections Radiofrequency ablation Intrathecal pumps Discography Vertebroplasty SI joint injection Back injections Spine stimulation Percutaneous discectomy Intradiscal treatments Stellate ganglion blockade. You might wonder what discomfort management medical professionals do that is different from your main care physician, and the response is a lot. The discomfort management field has actually grown throughout the years and continues to end up being more and more complex, making it that a lot more important to work with an expert.
While your primary care doctor is well-informed about a wide range of health and physical problems, they have actually not received the same level of training on particular conditions that an expert has actually gotten. In fact, in 2011 just 4 medical schools in the whole United States included courses that focused solely on discomfort in as a part of needed curriculum.
Part of what our pain management doctors do after medical school consists of finishing extra residencies, internships and fellowship training particular to the treatment of persistent pain. This additional training not just deepens their understanding of persistent pain itself, but also the interventional treatments that can assist reduce suffering and increase quality of life.
Our technique is to use the most ingenious and minimally intrusive approaches the industry needs to provide. To arrange a visit, find a place near you. how to establish a pain management clinic. Resources: Institute of Medication (United States) Committee on Advancing Pain Research Study, Care, and Education. Relieving Pain in America: A Blueprint for Changing Prevention, Care, Education, and Research study.
Pain management physicians physicians who focus on the examination, diagnosis, and treatment of discomfort have actually advanced training that qualifies them as your best source of treatment if you are experiencing any type of pain due to health problem or injury. After a basic residency, these doctors go through an additional one-year fellowship in pain management, and they are board-certified in a specialized, such as sport injuries or cancer pain.

See This Report about How Oftern Does A Pain Management Clinic Test Your Urine
Pain management physicians usually see patients with pain in the low back, knee, head, hip, and neck. Typical conditions dealt with is these doctors consist of: arthritis, fibromyalgia, migraines, sciatica, and more. For something, they diagnose the specific reason for your pain and the underlying conditions that lead to it.
It might be brought on by lots of conditions ranging from bad posture at your work desk to a herniated disc to a degenerative condition like arthritis. As soon as a discomfort management medical professional identifies your pain, he or she can find the therapy that works finest for you based on here their specialized training and the most recent research.
Discomfort doctors often use a large range of nonsurgical, interventional treatments along with complementary treatments as a method of minimizing the quantity of medication you require to take or to prevent the requirement for surgical treatment. These may consist of massage, a weight loss regimen, acupuncture, workout, yoga, meditation, physical treatment, dietary modifications, or chiropractic care.
Depending upon the intensity of your specific condition, they may likewise recommend epidural steroid injections, nerve blocks, joint injections, radiofrequency ablation, spine stimulation, or neuromodulation. If none of these techniques work in relieving your pain, surgical treatment might be an alternative of last hope. In any case, your discomfort management doctor will collaborate treatment between multiple medical professionals and healthcare experts.
Because function, your discomfort management physician serves as a supporter dedicated to alleviating your signs. For more information about how a discomfort management physician can assist you overcome your pain concerns, talk to the professionals at Pain Specialists of Austin and Central Texas Discomfort Center. We help patients like you every day.
All about What Drugs Are You Tested For At Pain Clinic
My partner and I pulled into the collapsing car park. It was only 9:30 a.m., but the parking area was nearly filled to capability with cars and trucks and individuals grating about and strolling in and out of the old structure, its signs hardly detectable. I had been retained to carry out an inspection of another medical practice under federal examination for issuing thousands of dosages of oxycodone "for aside from a genuine medical function." The entrance to the drug store on the very first floor of the building was manned by a guard, and neon-colored flyers littered the surrounding walls.
This was not a fantastic first impression. We waited on the elevator to the third floor, together with a half-dozen people in their mid-20s, early-30s. We stepped off the elevator and headed to Suite 322, and as expected, so did everybody else. Numerous individuals were seated on the floor in the corridor outside the medical suite and an older woman in a wheelchair was parked versus the wall.
In addition to the basic workplace waiting space chairs, several old collapsible chairs had actually also been brought in. There were no magazines, no side tables, simply a dusty floor light and some random medical leaflets inside a magazine rack bolted to the wall. It was clear that everybody had lacked persistence, people were grumbling and appeared to be competing for an award for who had been waiting the longest.
We stood in line at the reception counter behind a guy demanding to understand when 2 of his patients back there were going to be out. The receptionist had no response for him. The receptionist did not even take a look at me or my partner, she just handed me a new client consumption kind and told me to have a seat.
I discovered that somebody had actually currently pulled a couple lots patient charts and set up a card table in the evaluation room for us. The receptionist offered us coffee and stated the medical professional would be in to satisfy with us as quickly as she could. Right away, we observed the assessment space was barren.
The Main Principles Of How To File Complaint Against Pain Clinic
We took a seat and started to review the patient charts while we waited for the opportunity to interview our client regarding client care and practice policies. what depression screening should pain management clinic use. When the physician showed up for her interview, she began with her background and education-- she had actually just recently been hired to work locum tenens by the owner of the practice and had signed on for 6 months.
What Does Where North Of Boston Is There A Pain Clinic That Accepts Patients Eith No Insurance Mean?
Epidural injections Element injections Radiofrequency ablation Intrathecal pumps Discography Vertebroplasty SI joint injection Spine injections Spine stimulation Percutaneous discectomy Intradiscal treatments Stellate ganglion blockade. You might wonder what pain management medical professionals do that is various from your medical care doctor, and the answer is a lot. The pain management field has grown for many years and continues to end up being increasingly more complicated, making it that a lot more crucial to work with a professional.

While your medical care physician is knowledgeable about a wide array of health and physical concerns, they have actually not received the exact same level of training on specific conditions that a specialist has gotten. In reality, in 2011 just four medical schools in the whole United States included courses that focused exclusively on discomfort in as a part of needed curriculum.
Part of what our discomfort management medical professionals do after medical school includes completing extra residencies, internships and fellowship training specific to the treatment of chronic discomfort. This extra training not only deepens their understanding of persistent discomfort itself, but also the interventional procedures that can help minimize suffering and increase lifestyle.
Our approach is to use the most innovative and minimally invasive techniques the market has to offer. To set up an appointment, discover a location near you. my hospital is charging me 1727.00 for a urine test when i see pain clinic. Resources: Institute of Medicine (US) Committee on Advancing Pain Research Study, Care, and Education. Eliminating Pain in America: A Plan for Changing Prevention, Care, Education, and Research study.
Discomfort management medical professionals physicians who concentrate on the examination, diagnosis, and treatment of discomfort have advanced training that qualifies them as your finest source of treatment if you are experiencing any kind of pain due to disease or injury. After a basic residency, these doctors undergo an additional 1 year fellowship in pain management, and they are board-certified in a specialty, such as sport injuries or cancer pain.
What Are The Negatives Of Being Referred To A Pain Clinic Can Be Fun For Anyone
Pain management doctors usually see clients with discomfort in the low back, knee, head, hip, and neck. Typical conditions dealt with is these doctors consist of: arthritis, fibromyalgia, migraines, sciatica, and more. For something, they identify the particular cause of your discomfort and the hidden conditions that lead to it.
It might be triggered by numerous conditions ranging from poor posture at your work desk to a herniated disc to a degenerative condition like arthritis. When a discomfort management doctor diagnoses your discomfort, she or he can find the treatment that works best for you based upon their specialized training and the most recent research study.
Pain medical professionals typically utilize a large range of nonsurgical, interventional treatments along with complementary therapies as a way of reducing the amount of medication you require to take or to prevent the need for surgery. These might consist of massage, a weight loss routine, acupuncture, workout, yoga, meditation, physical therapy, dietary modifications, or chiropractic care.
Depending on the intensity of your specific condition, they may also recommend epidural steroid injections, nerve blocks, joint injections, radiofrequency ablation, back cable stimulation, or neuromodulation. If none of these approaches work in reducing your discomfort, surgery may be an alternative of last hope. In any case, your pain management doctor will collaborate treatment between numerous medical professionals and health care professionals.
In that role, your pain management physician functions as an advocate committed to relieving your symptoms. To read more about how a pain management physician can help you conquer your discomfort concerns, speak to the specialists at Pain Specialists of Austin and Central Texas Discomfort Center. We help clients like you every day.
How Do Kids Use The Skills That The Children's Pain Clinic Gives You Fundamentals Explained
My associate and I pulled into the collapsing parking lot. It was only 9:30 a.m., however the parking lot was nearly filled to capacity with cars and individuals milling about and strolling in and out of the old structure, its signage hardly noticeable. I had been kept to carry out an inspection of another medical practice under federal investigation for providing countless dosages of oxycodone "for other than a genuine medical purpose." The entryway to the pharmacy on the first flooring of the building was manned by a security guard, and neon-colored leaflets littered the surrounding walls.
This was not a fantastic first impression. We waited for the elevator to the third flooring, in addition to a half-dozen individuals in their mid-20s, early-30s. We stepped off the elevator and headed to Suite 322, and as expected, so did everyone else. Numerous people were seated on the flooring in the corridor outside the medical suite and an older woman in a wheelchair was parked against the wall.
In addition to the standard office waiting space chairs, numerous old collapsible chairs had actually also been brought in. There were no publications, no side tables, just a dusty floor light and some random medical leaflets inside a publication rack bolted to the wall. It was clear that everybody had actually lacked persistence, people were complaining and seemed to be contending for an award for who had been waiting the longest.
We stood in line at the reception counter behind a male requiring to understand when 2 of his patients back there were going to be out. The receptionist had no response for him. The receptionist did not even look at me or my associate, she just handed me a new patient consumption form and told me to have a seat.
I discovered that somebody had already pulled a couple dozen client charts and established a card table in the evaluation space for us. The receptionist used us coffee and said the medical professional would be in to meet with us as quickly as here she could. Right away, we noticed the evaluation room was barren.
The Basic Principles Of Who To Complain To About Pain Clinic
We sat down and started to review the client charts while we awaited the chance to interview our customer relating to client care and practice policies. what are the policies for prescribing opiates in a pain clinic in ny. When the doctor arrived for her interview, she began with her background and education-- she had just recently been worked with to work locum tenens by the owner of the practice and had signed on for 6 months.
The Main Principles Of What Is A Pain Management Clinic Nhs
Lots of doctors do drug screening and if they find you have too much in your system, they may assume you are abusing the drugs. Also, if you have insufficient of the drug in your system, they might believe you are selling the medication or providing it to someone else.
This specification is generally part of the arrangement due to the fact that medical professionals wish to ensure you are not abusing the drugs. They likewise desire to be sure you are the just one utilizing the medication. As an outcome, they arbitrarily evaluate you and then determine just how much of the drug is in your system.
It's not that they do not trust you or think that you are an addict. They might lose their medical license and face prosecution if they are recommending controlled compounds to individuals who are either abusing them or offering them to others. how long do you need to be off antibiotics before pain clinic shots. As a result, these agreements are designed to protect them.
They make this stipulation to keep clients from canceling due to the fact that they fear the drug test will expose that they are not taking their medications as prescribed (what i need for open a pain clinic office in ms). You consent to get all your prescriptions filled at one pharmacy, and you consent to enable the doctor and pharmacist to share details about you.
Because prescriptions are now participated in computer systems typically with interconnected databases, this practice is currently much more difficult to get away with. As a result, if you sign an agreement with your doctor, make certain you only shop at one pharmacy. You concur that lost, taken or ruined medications will not be changed.
Ensure nobody else has access to your medications. Preferably, opioid medications ought to be kept under lock and secret. There are some contracts that allow a physician to use his own discretion if your medication is taken and you file an authorities report. However keep in mind, he usually is not required to change the taken medication.
Rumored Buzz on How To Ask Pain Management Clinic For Pain Pills
You concur not to demand nor take pain medications from other health care companies. Even if you visit the dental professional or the emergency clinic, these medical professionals can not recommend pain medications for you. And, if they do, you will be violating your discomfort management arrangement. Only your pain management medical professional can prescribe discomfort medications.
As an outcome, if other physicians want to recommend medications for your injury or after dental surgery, they will require to go through your pain management doctor. Due to the drug tests you are taking, your discomfort management physician will be able to tell if you have taken something that he has actually not prescribed.
Normally, doctors who utilize these agreements state they are an efficient way to let clients understand what to anticipate while under their care - who are the names of pa's and np's at sanford pain clinic. They also think the contracts let patients understand how to utilize the medications safely, consisting of how to save them at house. However critics of the contracts stress that the contracts weaken the patient-doctor relationship.
They maintain that those with chronic pain are already susceptible and that the agreement moves the balance of power in favor of the medical professional, leaving the patient disempowered and at threat. Another concern is that the agreements are typically worded in a method that is offending to patients, which in turn produces bitterness in between the physician and the patient.
If you are asked to sign a discomfort management contract, it is essential that you comprehend every detail of what you are signing. By doing this, you will be able https://www.google.com/maps/d/edit?mid=1Z3RidvW8uLZc-tAPrfvS3qw_WvjfJLep&usp=sharing to follow all the rules and stipulations spelled out in the agreement. If you do not comprehend something, make certain to ask.
For https://www.google.com/maps/d/edit?mid=1fLhdYx-UPQwJH4rvueCuGuvAAquXAwj3&usp=sharing example, if you do not follow the arrangement or do something that is forbidden, your physician may refuse to recommend any extra discomfort medications for you. You also could be dismissed as a patient. And if you are dismissed, it can be much harder to discover another doctor to take you as a client and treat your condition.
Little Known Facts About How To Establish A Pain Management Clinic.
Ask questions about anything that is uncertain to you. Then, think about whether signing the agreement is the finest alternative for you. And if you do agree to sign the contract, make sure you follow it word for word. You do not want to find yourself in a circumstance where you can no longer get discomfort medications for your condition.
" One medical professional we went to described narcotics as the N-word," states Ann Jacobs, a client supporter for the American Discomfort Structure who looks after her chronically ill other half in Laramie, Wyo." [Doctor's] are so afraid of the DEA, scared of losing their license. So people go asking for pain relief." Many physicians are worried that there is a limitation on how much they can recommend in the course of their practice (legally there isn't), and if they fear their overall variety of prescriptions has gotten too expensive, they may cut down on refilling or writing brand-new prescriptions.

" This is genuine. We have actually had [patients] call where the doctor has actually fired them and will not even take their callsand that's it, out in the cold." It's a tricky balance. Medical professionals need to monitor their patients to ensure there's no wrongdoing, while patients with a genuine need wish to ensure a continuing supply of meds.
For a description of this practice, see Health.com's interview with leading pain expert, Russell K. Portenoy, MD. "You have to be there every thirty days, or you need to actually go there to get it refilled," says Cowan. "And sometimes if you miss one appointment, you have actually broken your agreement, and the physician says that's it, good-bye, no more." Andrea Cooper, 52, of Phoenix, Md., who suffers from fibromyalgia and spinal degeneration, https://www.google.com/maps/d/edit?mid=1HhEuTQykVUALfNDGYtzSZNcyY8_v3snS&usp=sharing has felt the preconception of narcotic usage.
There were indications up all over the office about rules and constraints. Everything about being suspicious of the clients. Not the way medication should be practiced. I discovered it insulting." Includes Jan, 45, a persistent pain patient in Boulder, Colo.: "I believe doctors need to be able to differentiate in between individuals who can handle it and those who ca n'tand help the people who can." If a doctor, for whatever reason, is unpleasant composing prescriptions for opioidswhether it's a brand-new prescription or a refillpatients can ask for a referral to a discomfort expert.
Experience a pain-free life once again with the assistance of Advocate Healthcare's leading discomfort management experts. Using the latest detection tools and treatment choices, our multi-disciplinary team will work with you to figure out the source of your pain and develop a thorough plan that fits your specific needs and objectives.
Some Of Where Is Northoaks Pain Management Clinic
To schedule a visit, callor. Neck and head discomfort Pain in the back Injuries to the spine, shoulders, knees and hips Element joint mediated pain Osteoarthritis and rheumatoid arthritis pain Neuropathic or nerve discomfort Facet joint moderated neck or back discomfort Intricate regional pain syndrome Job-related and sports-related discomfort Surgical discomfort Cancer pain Shingles discomfort Fibromyalgia Post herpetic neuralgia Degenerative disc illness Spine compression fractures Spine stenosis Sciatica/ herniated disc Through substantial experience, Advocate understands that reducing pain is accomplished best through a collaborative effort between discomfort management professionals, primary care physicians and the patients themselves.
The 9-Minute Rule for What Goes Into A Time Duration Executive Milestone For A Pain Management Clinic
Many physicians do drug testing and if they find you have too much in your system, they might presume you are abusing the drugs. Likewise, if you have too little of the drug in your system, they might believe you are offering the medication or giving it to another person.
This specification is typically part of the agreement since medical professionals desire to guarantee you are not abusing the drugs. They also desire to be sure you are the just one using the medication. As a result, they arbitrarily test you and after that measure just how much of the drug remains in your system.
It's not that they do not trust you or believe that you are a drug addict. They might lose their medical license and face criminal prosecution if they are recommending illegal drugs to people who are either abusing them or selling them to others. what is a pain clinic uk. As a result, these arrangements are developed to secure them.
They make this terms to keep clients from canceling because they fear the drug test will reveal that they are not taking their medications as recommended (how to get prescribed roxicodone from my pain clinic). You consent to get all your prescriptions filled at one drug store, and you accept permit the doctor and pharmacist to share details about you.
Due to the fact that prescriptions are now gotten in into computers typically with interconnected databases, this practice is presently much more tough to get away with. Consequently, if you sign a contract with your physician, make sure you only store at one drug store. You agree that lost, stolen or damaged medications will not be replaced.
Make sure no one else has access to your medications. Preferably, opioid medications must be kept under lock and secret. There are some agreements that allow a physician to utilize his own discretion if your medication is taken and you submit an authorities report. However keep in mind, he generally is not required to replace the taken medication.
The Ultimate Guide To How Does A Pain Management Clinic Help People
You agree not to request nor take discomfort medications from other health care suppliers. Even if you go to the dental practitioner or the emergency space, these doctors can not prescribe pain medications for you. And, if they do, you will be breaking your discomfort management contract. Just your discomfort management doctor can prescribe discomfort medications.
As an outcome, if other medical professionals want to prescribe medications for your injury or after oral surgical treatment, they will need to go through your discomfort management physician. Due to the drug tests you are taking, your discomfort management physician will have the ability to inform if you have taken something that he has not recommended.
Generally, physicians who utilize these agreements say they are an efficient method to let clients know what to expect while under their https://www.google.com/maps/d/edit?mid=1HhEuTQykVUALfNDGYtzSZNcyY8_v3snS&usp=sharing care - how to open a pain management clinic in florida. They likewise believe the contracts let patients understand how to utilize the medications safely, including how to keep them at house. However critics of the arrangements worry that the contracts weaken https://www.google.com/maps/d/edit?mid=1fLhdYx-UPQwJH4rvueCuGuvAAquXAwj3&usp=sharing the patient-doctor relationship.
They maintain that those with persistent pain are currently vulnerable and that the contract moves the balance of power in favor of the medical professional, leaving the client disempowered and at threat. Another issue is that the contracts are frequently worded in such a way that is offensive to clients, which in turn creates bitterness in between the medical professional and the patient.
If you are asked to sign a discomfort management agreement, it is vital that you comprehend every information of what you are signing. In this manner, you will have the ability to comply with all the guidelines and specifications defined in the contract. If you do not comprehend something, make sure to ask.
For instance, if you do not follow the agreement or do something that is prohibited, your medical professional might refuse to prescribe any additional pain medications for you. You likewise could be dismissed as a patient. And if you are dismissed, it can be much harder to discover another physician to take you as a patient and treat your condition.
What Does A Pain Management Clinic Do Can Be Fun For Anyone
Ask concerns about anything that is unclear to you. Then, think of whether signing the contract is the best alternative for you. And if you do concur to sign the contract, make sure you follow it word for word. You don't desire to find yourself in a scenario where you can no longer get pain medications for your condition.
" One doctor we went to described narcotics as the N-word," says Ann Jacobs, a client advocate for the American Discomfort Structure who takes care of her chronically ill partner in Laramie, Wyo." [Medical professional's] are so fearful of the DEA, terrified of losing their license. So people go asking for discomfort relief." Lots of doctors are concerned that there is a limitation on how much they can recommend in the course of their practice (lawfully there isn't), and if they fear their total variety of prescriptions has actually gotten expensive, they may cut down on refilling or writing new prescriptions.
" This is real. We have actually had [clients] call where the medical professional has fired them and will not even take their callsand that's it, out in the cold." It's a tricky balance. Doctors need to monitor their patients to ensure there's no wrongdoing, while patients with a legitimate need wish to guarantee a continuing supply of medications.
For an explanation of this practice, see Health.com's interview with leading discomfort expert, Russell K. Portenoy, MD. "You need to be there every 1 month, or you have to actually go there to get it filled up," says Cowan. "And in some cases if you miss one appointment, you've broken your agreement, and the physician states that's it, good-bye, no more." Andrea Cooper, 52, of Phoenix, Md., who struggles with fibromyalgia and spine degeneration, has actually felt the preconception of narcotic usage.
There were register all over the office about rules and restrictions. All about being suspicious of the patients. Not the method medicine ought to be practiced. I discovered it insulting." Includes Jan, 45, a chronic pain sufferer in Boulder, Colo.: "I believe medical professionals need to have the ability to compare the people who can handle it and those who ca n'tand assist individuals who can." If a physician, for whatever factor, is uncomfortable composing prescriptions for opioidswhether it's a brand-new prescription or a refillpatients can ask for https://www.google.com/maps/d/edit?mid=1Z3RidvW8uLZc-tAPrfvS3qw_WvjfJLep&usp=sharing a recommendation to a discomfort specialist.
Experience a pain-free life as soon as again with the assistance of Advocate Healthcare's leading pain management specialists. Using the newest detection tools and treatment choices, our multi-disciplinary team will deal with you to figure out the source of your pain and create a thorough plan that fits your particular requirements and goals.
The Greatest Guide To What Disease Is The Estimated Cost For A Free-standing Pain Clinic
To schedule an appointment, callor. Neck and head pain Pain in the back Injuries to the spinal column, shoulders, knees and hips Aspect joint moderated pain Osteoarthritis and rheumatoid arthritis pain Neuropathic or nerve pain Element joint mediated neck or pain in the back Complicated regional discomfort syndrome Work-related and sports-related pain Surgical pain Cancer discomfort Shingles pain Fibromyalgia Post herpetic neuralgia Degenerative disc disease Back compression fractures Back stenosis Sciatica/ herniated disc Through extensive experience, Advocate understands that reducing discomfort is accomplished best through a collective effort in between discomfort management specialists, medical care physicians and the patients themselves.
The smart Trick of When Was The First Pain Management Clinic Was Opened That Nobody is Talking About
Many physicians do drug testing and if they discover you have excessive in your system, they may presume you are abusing the drugs. Similarly, if you have too little of the drug in your system, they might think you are offering the medication or offering it to somebody else.
This stipulation is usually part of the agreement due to the fact that doctors wish to guarantee you are not abusing the drugs. They likewise want to be sure you are the only one using the medication. As a result, they randomly evaluate you and then measure how much of the drug remains in your system.
It's not that they do not trust you or believe that you are a druggie. They could lose their medical license and face criminal prosecution if they are recommending illegal drugs to people who are either abusing them or offering them to others. what is pain management clinic. As an outcome, these contracts are designed to secure them.
They make this terms to keep patients from canceling due to the fact that they fear the drug test will expose that they are not taking their medications as prescribed (how oftern does a pain management clinic test your urine). You consent to get all your prescriptions filled at one drug store, and you consent to enable the doctor and pharmacist to share info about you.
Due to the fact that prescriptions are now participated in computer systems often with interconnected databases, this practice is currently much more tough to get away with. As a result, if you sign a contract with your doctor, make certain you only store at one drug store. You concur that lost, stolen or damaged medications will not be replaced.
Ensure nobody else has access to your medications. Ideally, opioid medications ought to be kept under lock and key. There are some arrangements that enable a medical professional to use his own discretion if your medication is taken and you file a police report. However remember, he usually is not required to replace the taken medication.
All about Who To Complain To About Pain Clinic
You concur not to demand nor take pain medications from other health care suppliers. Even if you go to the dental expert or the emergency room, these doctors can not recommend pain medications for you. And, if they do, you will be breaching your discomfort management agreement. Just your pain management doctor can recommend discomfort medications.
As a result, if other physicians wish to recommend medications for your injury or after dental surgery, they will need to go through your discomfort management medical professional. Due to the drug tests you are taking, your discomfort management physician will have the ability to inform if you have taken something that he has actually not prescribed.
Normally, physicians who use these contracts state they are an effective way to let clients understand what to expect while under their care - who are the names of pa's and np's at sanford pain clinic. They likewise believe the agreements let clients understand how to use the medications securely, consisting of how to save them at home. However critics of the arrangements worry that the agreements undermine the patient-doctor relationship.
They preserve that those with persistent pain are already vulnerable which the arrangement moves the balance of power in favor of the physician, leaving the patient disempowered and at risk. Another issue is that the contracts are often worded in such a way that is offending to clients, which in turn creates bitterness between the medical professional and the client.
If you are asked to sign a pain management arrangement, it is necessary that you comprehend every detail of what you are https://www.google.com/maps/d/edit?mid=1HhEuTQykVUALfNDGYtzSZNcyY8_v3snS&usp=sharing signing. By doing this, you will be able to comply with all the guidelines and specifications spelled out in the contract. If you do not understand something, make certain to ask.
For instance, if you do not follow the arrangement or do something that is prohibited, your doctor might decline to prescribe any extra pain medications for you. You also might be dismissed as a client. And if you are dismissed, it can be much harder to find another medical professional to take https://www.google.com/maps/d/edit?mid=1Z3RidvW8uLZc-tAPrfvS3qw_WvjfJLep&usp=sharing you as a client and treat your condition.
Why Do Patients Have To Go Through Pain Clinic To Get Pain Meds Things To Know Before You Buy
Ask questions about anything that is uncertain to you. Then, consider whether signing the arrangement is the very best choice for you. And if you do accept sign the agreement, make sure you follow it word for word. You don't wish to discover yourself in a circumstance where you can no longer get discomfort medications for your condition.

" One medical professional we went to described narcotics as the N-word," states Ann Jacobs, a patient supporter for the American Discomfort Structure who cares for her chronically ill spouse in Laramie, Wyo." [Medical professional's] are so fearful of the DEA, scared of losing their license. So individuals go asking for pain relief." Lots of physicians are worried that there is a limit on just how much they can recommend in the course of their practice (legally there isn't), and if they fear their total variety of prescriptions has gotten expensive, they may cut back on refilling or writing new prescriptions.
" This is real. We've had [clients] call where the medical professional has fired them and won't even take their callsand that's it, out in the cold." It's a https://www.google.com/maps/d/edit?mid=1fLhdYx-UPQwJH4rvueCuGuvAAquXAwj3&usp=sharing challenging balance. Physicians need to monitor their clients to ensure there's no misdeed, while clients with a genuine need want to guarantee a continuing supply of medications.
For an explanation of this practice, see Health.com's interview with leading pain expert, Russell K. Portenoy, MD. "You need to exist every one month, or you have to really go there to get it filled up," says Cowan. "And in some cases if you miss out on one visit, you have actually broken your contract, and the medical professional states that's it, good-bye, no more." Andrea Cooper, 52, of Phoenix, Md., who experiences fibromyalgia and spine degeneration, has actually felt the preconception of narcotic usage.
There were indications up all over the workplace about rules and restrictions. All about being suspicious of the clients. Not the method medicine ought to be practiced. I found it insulting." Adds Jan, 45, a chronic pain patient in Boulder, Colo.: "I think medical professionals need to be able to distinguish between individuals who can manage it and those who ca n'tand help the people who can." If a doctor, for whatever factor, is uncomfortable composing prescriptions for opioidswhether it's a new prescription or a refillpatients can request a referral to a pain professional.
Experience a pain-free life once again with the assistance of Advocate Healthcare's leading pain management experts. Utilizing the current detection tools and treatment options, our multi-disciplinary group will deal with you to figure out the source of your discomfort and create a detailed plan that fits your specific needs and objectives.
What Does What Does The Pain Clinic Do Mean?
To set up an appointment, callor. Neck and head discomfort Neck and back pain Injuries to the spine, shoulders, knees and hips Facet joint moderated discomfort Osteoarthritis and rheumatoid arthritis pain Neuropathic or nerve pain Element joint moderated neck or back pain Complicated regional discomfort syndrome Job-related and sports-related discomfort Surgical discomfort Cancer pain Shingles pain Fibromyalgia Post herpetic neuralgia Degenerative disc disease Spine compression fractures Spine stenosis Sciatica/ herniated disc Through extensive experience, Advocate understands that easing discomfort is achieved best through a collective effort between pain management professionals, medical care doctors and the patients themselves.
Clinic How To Tell If Someone Is In Pain Or Trying To Get Pain Meds Fundamentals Explained
If you live with persistent discomfort, you likely require a group of physicians to achieve an optimal outcome. Here's what to get out of a discomfort specialty practice or center. So you have actually chosen it's time to make a consultation with a discomfort physician, or at a discomfort center. Here's what you need to understand prior to scheduling your visitand what to expect once you're there.
" Pain doctors originate from many different academic backgrounds," states Dmitry M. Arbuck, MD, president and medical director of the Indiana Polyclinic in Indianapolis, a discomfort management center. Dr. Arbuck is accredited by the American Academy of Discomfort Management and the American Board of Psychiatry and Neurology. "Any medical professional from any specialtyfor instance, emergency situation medicine, household practice, neurologymay be a discomfort physician." The pain physician you see will depend upon your symptoms, medical diagnosis, and requires.
Arbuck explains. "The physicians within a discomfort management clinic or practice might specialize in rheumatology, orthopedics, gastroenterology, psychiatry," or other areas, for example. Discomfort physicians have made the title of MD (Medical Professional of Medication) or DO (Medical Professional of Osteopathic Medication). Some discomfort doctors are fellowship-trained, indicating they received post-residency training in this sub-specialty.
( Find out more about interventional pain techniques.) Pain physicians who have met certain qualificationsincluding finishing a residency or fellowship and passing a composed examare thought about to be board-certified. Many pain medical professionals are dual-board certified in, for example, anesthesiology and palliative medicine. However, not all pain physicians are board-certified or have formal training in discomfort medication, however that doesn't mean you shouldn't consult them, says Dr.
Things about How Does A Pain Management Clinic Help People
Dr. Arbuck advises that people seeking help for chronic discomfort see physicians at a center or a group practice since "nobody specialist can truly treat pain alone." He discusses, "You don't wish to choose a certain type of physician, necessarily, but a good physician in an excellent practice."" Discomfort practices should be multi-specialty, with a great credibility for utilizing more than one technique and the ability to attend to more than one problem," he recommends. what pain clinic will give you roxy 15th for back pain.
As Dr. Arbuck describes, "If you have one doctor or specialized that's more crucial than the others," the treatment that specialized prefers will be stressed, and "other treatments may be neglected." This design can be problematic because, as he explains: "One pain patient may require more interventions, while another might require a more mental technique." And because pain clients also benefit from multiple therapies, they "need to have access to doctors who can refer them to other experts in addition to work with them." Another benefit of a multi-specialty discomfort practice or clinic is that it helps with regular multi-specialty case conferences, in which all the physicians meet to go over patient cases.
Arbuck points out. Believe of it like a board meetingthe more that members with different backgrounds collaborate about an individual challenge, the more likely they are to solve that particular problem. At a pain center, you might also consult with physical therapists (OTs), physiotherapists (PTs), qualified physician's assistants (PA-C), nurse practitioners (NPs), certified acupuncturists (LAc), chiropractics physician (DC), and workout physiologists.
The latter are frequently social employees, with titles such as certified medical social employee (LCSW). Dr. Arbuck views reliable pain medication as a spectrum of services, with mental treatment on one end and interventional discomfort management on the other. In in between, clients are able to get a combination of pharmacological and corrective services from different doctors and other doctor.
Getting The How To Get Into A Pain Clinic To Work
Preliminary visits might include several of the following: a physical examination, interview about your medical history, discomfort evaluation, and diagnostic tests or imaging (such as x-rays). In addition, "A great multi-specialty center will pay equal attention to medical, psychiatric, surgical, family, addiction, and social history. That's the only way to examine patients thoroughly," Dr.
At the Indiana Polyclinic, for example, clients have the opportunity to consult professionals from four main areas: This may be an internist, neurologist, household specialist, and even a rheumatologist. This physician normally has a large knowledge of a broad medical specialty. This physician is likely to be from a field that where interventions are frequently used to treat pain, such as anesthesiology.
This company will be somebody who specializes in the function of the body, such as a physical medication and rehabilitation (PM&R) doctor, physical therapist, physical therapist, or chiropractor. Depending on the patient, he or she might likewise see a psychiatrist, psychologist, and/or psychotherapist. The patient's medical care physician may collaborate care.
Arbuck. "Narcotics are just one tool out of many, and one tool can not work at perpetuity." Additionally, he notes, "pain clinics are not simply puts for injections, nor is discomfort management almost psychology. The objective is to come to visits, and follow through with rehab programs. Pain management is a dedication.
What Was The First Pain Management Clinic Things To Know Before You Buy

Arbuck points out. Treatment can be costly and due to the fact that of that, patients and medical professional's workplaces frequently require to eliminate for medications, visits, and tests, but this difficulty takes place beyond pain clinics as well. read more Patients need to likewise understand that anytime controlled compounds (such as opioids) are associated with a treatment strategy, the doctor is going to demand drug screenings and Patient Contract forms regarding rules to follow for safe dosingboth are recommended by federal agencies such as the FDA (see a sample Patient-Prescriber Opioid Contract at https://www.fda.gov/media/114694/download).
" I didn't just have discomfort in my head, it was in the neck, jaw, absolutely all over," remembers the HR professional, who lives in the Indianapolis area - what medication in clinic abdominal pain. Wendy started seeing a neurologist, who put her on high doses of the anti-seizure medications gabapentin and zonisamide for discomfort relief. Sadly, she says, "The pain worsened, and the negative effects from the medication left me not able to https://www.wfxg.com/story/42141829/addiction-treatment-center-in-miami-educates-community-about-drug-rehab functionI had amnesia, blurred vision, and muscle weak point, and my face was numb.
Wendy's neurologist provided her Botox injections, however these caused some hearing and vision loss. She also tried acupuncture and even had a pain relief gadget implanted in her lower back (it has given that been removed). Lastly, after 12 years of extreme, chronic pain, Wendy was referred to the Indiana Polyclinic.

She likewise went through various evaluations, including an MRI, which her previous medical professional had performed, along with allergic reaction and hereditary testing. From the latter, "We found out that my system does not take in medication appropriately and pain medications are not reliable." Shortly afterwards, Wendy got some unexpected news: "I discovered I didn't have chronic migraine, I had trigeminal neuralgia." This condition provides with signs of severe discomfort in the facial location, triggered by the brain's three-branched trigeminal nerve.
The Best Guide To How Pelvic Pain Exam Done In Minute Clinic
Wendy began getting nerve blocks from the center's anesthesiologist. She gets 6 shots of lidocaine (a local anesthetic) and an anti-inflammatory to her forehead and cheeks. "It's five minutes of unbearable discomfort for 4 months of relief," Wendy shares. She likewise seized the day to deal with the clinic's discomfort psychologist twice a month, and the occupational therapist once a month.
The Single Strategy To Use For Who Runs The Va Hospital Pain Clinic Lexington Ky
The listing will provide an address and contact number (in addition to any disciplinary actions appointed to the physician). A group of local pain experts, the, have come together to help in case a pain clinic unexpectedly closes and clients discover themselves unexpectedly without access to care or suggestions.
Nevertheless, the group believes that we should come together as a community to help our next-door neighbors when they, by no fault of their own, suddenly find themselves medically orphaned due to the sudden closure of their pain center. Kentuckiana toll complimentary number: Note: This toll free number is not manned.
It is not a general referral service for patients. And there is no assurance you will get a call back. If you believe you may have a medical emergency, call your doctor, go to the emergency situation department, or call 911 right away. This blog site post will be upgraded with, lists, contact number, and extra resources when brand-new info appears.
And don't quit hope. This circumstance might be hard, but it may also be a chance for a brand-new beginning. * Note: All clinicians need to be familiar with the info in Part One (above) as this is what your patients read. Primary Care practices will likely shoulder the majority of continuity of care issues caused by the unexpected closure of https://how-much-is-an-8-ball-of-cocaine.drug-rehab-florida-guide.com/ a large discomfort center.
3 questions end up being vital: Do you continue the existing routine? Do you alter the program (e.g. taper or devise a new plan)? Do you choose not to recommend any medications and deal with the withdrawal? The answers to these questions can just come from the private care service provider. Naturally, we want to minimize suffering.
The Main Principles Of What Was The First Pain Management Clinic
Some prescribers may feel comfy with greater dosages and specialized solutions of medications. Others may be prepared to prescribe (within a narrower set of individual borders) frequently recommended medications with which they have familiarity. And there will be some clinicians who honestly feel they are not equipped (i.e. training, experience, manpower) to prescribe illegal drugs at all.
Let's begin with some suggestions from the Washington State Department of Health (a leader in dealing with opioid prescribing problems): Clinicians ought to empathically evaluate benefits and dangers of ongoing high-dosage opioid treatment and deal to deal with the patient to taper opioids to lower dosages. Specialists keep in mind that patients tapering opioids after taking them for many years may require extremely slow opioid tapers along with pauses in the taper to allow steady accommodation to lower opioid dosages - what is a pain clinic and what do they do.
The U.S. Centers for Illness Control and Prevention specifically encourages against quick taper for individuals taking more than 90 mg MEDICATION per day. Clinicians must evaluate patients on more than 90 mg MED or who are on mix therapy for overdose threat. Recommend or provide naloxone. More on this subject is in the New England Journal of Medicine.
Pharmacist keeping in mind different withdrawal metrics: Frequently a lower dose than they are accustomed to taking will suffice. for dealing with opioid withdrawal is to calculate the patient's (morphine comparable daily dosage) and after that supply the client with a portion of this MEDD (e.g. 80-90%), in the form of immediate release medication, for a few days and then re-evaluate.
Instead the clinician may recommend opioids with which he or she feels more comfy (i.e. Percocet rather of Oxycontin) and still treat the client's withdrawal effectively. Fortunately, there are a variety of well-vetted procedures to guide us. An effective plan of care is born of understanding about the patient (e.g.
Some Ideas on What Does A Pain Clinic Do You Should Know
The Mayo Center published a terrific fundamental guide on opioid tapering: And the Washington State Company Medical Directors' Group has a very great step-by-step guide to tapering: For medical care suppliers who do not wish to compose the medications, they may need to handle treating withdrawal. I found an exceptional and easy to use guide to treating opioid withdrawal in (and other medications in other chapters) from the As kept in mind above in Part One, the has actually published a concise "pocket guide" to tapering.
Ref: https://www.cdc - what to expect at a pain management clinic.gov/drugoverdose/pdf/clinical_pocket_guide_tapering-a.pdf Reasonably, even the most diligent tapering strategies can miss out on the mark, and withdrawal symptoms of differing severity can occur. Likewise, as specified above, some clinicians will make the decision to recommend any regulated substances in treatment of their clients' withdrawal. In either instance, clinicians require to be knowledgeable about what is readily available (over the counter as well as by prescription) to deal with withdrawal symptoms.
And for those clinicians interested some of the more intense pharmacologic techniques to treating withdrawal, consider this post from Dialogues in Scientific Neuroscience: Excerpts:: The antihypertensive, 2-adrenergic agonist drug clonidine has been used to facilitate opioid withdrawal in both inpatient and outpatient settings for over 25 years.18 21 It works by binding to 2 autoreceptors in the locus coeruleus and suppressing its hyperactivity during withdrawal.
Dropouts are most likely to take place early with clonidine and later on with methadone. In a study of heroin detoxing, buprenorphine did better on retention, heroin use, and withdrawal seriousness than the clonidine group.12 Because clonidine has mild analgesic effects, added analgesia might not be required throughout the withdrawal period for medical opioid addicts.
Lofexidine, an analogue of clonidine, has been approved in the UK and may be as effective as clonidine for opioid withdrawal with less hypotension and sedation.23,24 Combining lofexidine with low-dose naloxone appears to enhance retention signs and time to relapse. Encouraging measures: Sleeping disorders is both typical and incapacitating. Clonazepam, trazodone, and Zolpidem have all been utilized for withdrawal-related insomnia, however the decision to utilize a benzodiazepine needs to be made carefully, particularly for outpatient cleansing. Vitamin and mineral supplements are frequently offered.
Getting My Why Do Patients Have To Go Through Pain Clinic To Get Pain Meds To Work

A note on regulations: When recommending, remember that Kentucky now has enforced a three-day limitation for treatment of acute conditions with Set up II illegal drugs. If your client has chronic discomfort, and your treatment addresses this persistent condition, then the three-day limitation ought to not use. Here is the language in Kentucky's discomfort regulations: In addition to the other requirements established in this administrative policy, for functions of dealing with pain as or associated to an intense medical condition, a doctor shall not prescribe or give more than a 3 (3 )day supply of an Arrange II illegal drug, unless the physician determines that more than a 3 (3) day supply is medically essential and the doctor documents the acute medical condition and absence of alternative medical treatment choices to validate the quantity of the regulated compound prescribed or dispensed. The mnemonic" Plan to THINK" (see listed below) can assist physicians remember what Kentucky needs in order to initially recommend controlled compounds for chronic discomfort: File a plan() that explains why and how the regulated compound will be used. Teach() the patient about proper storage of the medications and when to stop taking them (where is northoaks pain management clinic).
Excitement About What Will A Pain Clinic Do For Me
The listing will provide an address and telephone number (in addition to any disciplinary actions appointed to the physician). A group of regional pain experts, the, have actually come together to help in case a discomfort clinic suddenly closes and patients find themselves unexpectedly without access to care or advice.
Nevertheless, the group believes that we should come together as a neighborhood to help our neighbors when they, by no fault of their own, suddenly discover themselves clinically orphaned due to the sudden closure of their pain clinic. Kentuckiana toll free number: Note: This toll free number is not manned.
It is not a basic recommendation service for patients. And there is no assurance you will get a call back. If you believe you may have a medical emergency, call your medical professional, go to the emergency department, or call 911 right away. This blog site post will be upgraded with, lists, telephone number, and additional resources when brand-new information ends up being readily available.
And don't offer up hope. This situation might be hard, but it may likewise be an opportunity for a clean slate. * Note: All clinicians should be familiar with the info in Part One (above) as this is what your clients are checking out. Medical care practices will likely shoulder the bulk of connection of care issues produced by the abrupt closure of a big discomfort clinic.
Three questions end up being paramount: Do you continue the existing program? Do you change the routine (e.g. taper or create a new plan)? Do you decide not to prescribe any medications and handle the withdrawal? The responses to these questions can just come from the private care supplier. Obviously, we desire to ease suffering.
Fascination About What Is The Estimated Cost To Building A Free-standing 8 Hour A Day Pain Clinic
Some prescribers might feel comfy with higher doses and specialized formulations of medications. Others may want to prescribe (within a narrower set of personal limits) typically prescribed medications with which they have familiarity. And there will be some clinicians who honestly feel they are not geared up (i.e. training, experience, workforce) to prescribe illegal drugs at all.
Let's start with some suggestions from the Washington State Department of Health (a leader in resolving opioid recommending issues): Clinicians need to empathically review advantages and risks of ongoing high-dosage opioid treatment and deal to deal with the client to taper opioids to lower dosages. Professionals note that patients tapering opioids after taking them for several years may require really slow opioid tapers as well as stops briefly in the taper to allow gradual lodging to lower opioid does - how to open a pain management clinic in florida.
The U.S. Centers for Illness Control and Avoidance particularly encourages against quick taper for individuals taking more than 90 mg MED daily. Clinicians ought to evaluate patients on more than 90 mg MEDICATION or who are on mix treatment for overdose threat. Recommend or offer naloxone. More on this subject is in the New England Journal of Medication.
Pharmacist keeping in mind various withdrawal metrics: Frequently a lower dose than they are accustomed to taking will suffice. for dealing with opioid withdrawal is to calculate the patient's (morphine comparable daily dose) and then supply the patient with a portion of this MEDD (e.g. 80-90%), in the kind of instant release medication, for a few days and after that re-evaluate.
Rather the clinician might prescribe opioids with which he or she feels more comfy (i.e. Percocet instead of Oxycontin) and still deal with the client's withdrawal successfully. Fortunately, there are a variety of well-vetted procedures to direct us. An effective strategy of care is born of knowledge about the patient (e.g.
Not known Facts About How Do You Get Into A Pain Management Clinic
The Mayo Clinic published an excellent basic guide on opioid tapering: And the Washington State Company Medical Directors' Group has an extremely nice detailed guide to tapering: For primary care companies who do not wish to compose the medications, they might need to deal with treating withdrawal. I found an excellent and simple to utilize guide to dealing with opioid withdrawal in (and other medications in other chapters) from the As noted above in Part One, the has released a succinct "pocket guide" to tapering.
Ref: https://www.cdc - how to get prescribed roxicodone from my pain clinic.gov/drugoverdose/pdf/clinical_pocket_guide_tapering-a.pdf Reasonably, even the most diligent tapering strategies can miss out on the mark, and withdrawal symptoms of differing seriousness can occur. Likewise, as stated above, some clinicians will make the choice to recommend any regulated compounds in treatment of their patients' withdrawal. In either circumstances, clinicians require to be knowledgeable about what is available (non-prescription in addition to by prescription) to treat withdrawal signs.
And for those clinicians intrigued some of the more extreme pharmacologic techniques to dealing with withdrawal, consider this post from Dialogues in Medical Neuroscience: Excerpts:: The antihypertensive, 2-adrenergic agonist drug clonidine has been used to help with opioid withdrawal in both inpatient and outpatient settings for over 25 years.18 21 It works by binding to 2 autoreceptors in the locus coeruleus and reducing its hyperactivity during withdrawal.
Dropouts are most likely to happen early with clonidine and later with methadone. In a research study of heroin detoxification, buprenorphine did much better on retention, heroin use, and withdrawal intensity than the clonidine group.12 Given that clonidine has moderate analgesic effects, included analgesia may not be needed throughout the withdrawal duration for medical opioid addicts.
Lofexidine, an analogue of clonidine, has actually been authorized in the UK and may be as reliable as clonidine for opioid withdrawal with less hypotension and sedation.23,24 Combining lofexidine with low-dose naloxone appears to enhance retention symptoms and time to relapse. Encouraging measures: Sleeping disorders is both typical and incapacitating. Clonazepam, trazodone, and Zolpidem have all been used for withdrawal-related insomnia, but the decision to utilize a benzodiazepine needs to be made thoroughly, particularly for outpatient detoxing. Minerals and vitamin supplements are often offered.
Things about How To Open A Pain Management Clinic
A note on regulations: When prescribing, keep in mind that Kentucky now has imposed a three-day limitation for treatment of severe conditions with Arrange II illegal drugs. If your patient has persistent pain, and your treatment addresses this chronic condition, then the three-day limitation should not use. Here is the language in Kentucky's pain guidelines: In addition to the other standards established in this administrative guideline, for purposes of dealing with discomfort as or associated to an intense medical condition, a doctor will not prescribe or dispense more than a 3 (3 )day supply https://how-much-is-an-8-ball-of-cocaine.drug-rehab-florida-guide.com/ of an Arrange II controlled compound, unless the physician identifies that more than a three (3) day supply is clinically required and the physician records the acute medical condition and absence of alternative medical treatment alternatives to validate the quantity of the regulated substance prescribed or dispensed. The mnemonic" Strategy to THINK" (see below) can assist physicians remember what Kentucky needs in order to initially recommend illegal drugs for chronic discomfort: Document a strategy() that describes why and how the illegal drug will be used. Teach() the client about correct storage of the medications and when to stop taking them (what to do when pain clinic does not prescribe meds you need).
What's The Difference Between A Hospital And A Clinic? - Quora Can Be Fun For Everyone
Table of ContentsThe 9-Minute Rule for Clinic - Description, Types, & Function - BritannicaClinic Vs. Hospital - Blog - Amopportunities Can Be Fun For AnyoneUnknown Facts About Clinic - Definition Of Clinic By Medical DictionaryThe Only Guide to Hospital-based Outpatient ClinicClinic - Definition Of Clinic At Dictionary.com - The FactsThe Definitive Guide for What's The Difference Between A Hospital And A Clinic? - Quora
I would much rather you review the labs, identify that the cbc was typical, and after that simply point out "normal CBC" in the note. Likewise, if a research study is abnormal, consider what particular components are awry, and highlight them, which ought to present the data in a workable/usable format. It might take experience/practice before you find out what it relevanat (and why), however a minimum of the above system will require you to believe! Some computer system record systems make it possible to "cut and paste" another clinician's history into your note.
There are lots of methods of approaching medical problems. You may discover it useful, especially when dealing with intricate medical issues, to break each issue into its a lot of fundamental components, with a separate plan kept in mind for each one. By recognizing the a lot of standard components of each problem, you will be less likely to miss essential problems and be much better able to create the most inclusive/complete strategy possible.
Nevertheless, this general technique uses to most medical circumstances. Let's take, for instance, a patient who provides with brand-new dyspnea on exertion who also has understood coronary artery illness, CHF, high blood pressure and hyperlipidemia. Every one of these problems is associated with the patient's cardiovascular system. Nevertheless, if you were to address all of them under a single "cardiovascular" heading, there is a great opportunity that the assessment and plan would end up being jumbled and complicated.
9 Simple Techniques For What Is The Purpose Of Clinic? — Dankmeyer, Inc.
No symptoms of angina (which was related to left-sided chest pain in the past). No workout induced desaturation kept in mind during observed 3 minute walk in center. Nothing on examination to suggest CHF. Patient Visit this website has considerable cigarette smoking history, though not understood to have COPD, and no existing wheezing on exam (no past PFTs).
Etiology of dyspnea not clear. In any case, not clearly disabled by signs. Acquire PFTs Acquire CXR today CBC to r/o anemia as cause Re-Evaluate in clinic in 6 w (or patient will call quicker if symptoms get worse) ... at that time will consider repeat Workout Tolerance Test to asses for ischemia/quantify exercise tolerance; likewise think about repeat echo to reassess LV function.
Patient continues to be active without symptoms. Continue aspirin and lopressor (beta blocker) Patient knowledgeable about signs suggestive of persistent ischemia. If accompany activity, will repeat Workout Tolerance Test. CHF: Understood depressed left ventricular function on basis previous MI, with EF 30% by last echo. No signs for over 1 year considering that initiation of medical treatment.
The Ultimate Guide To Is A Post-discharge Clinic In Your Hospital's Future? - The ...
End organ dysfunction (CHF and CAD) handled as above. Continue medical treatment as above Hyperlipidemia: LDL 80, HDL 40 both at target levels on Simvastatin (HMG-COA Reductase Inhibitor) 20 mg/d. Continue Simvastatin at present dose Inspect parenchymal liver enzymes (alt/ast), Creatinine Kinase today and in 6 months to ensure no toxicity.
This consists of age and sex specific screening tests in addition to vaccinations that are otherwise simple to over look. For males this would include (roughly ... the following are not always the definitive guidelines): Factor to consider for examining PSA (African-Americans beginning age over 40; Others over 50) Colorectal cancer screening (age over 50 and every 5-10 years afterwards) For ladies: Yearly PAP smear (beginning at age of sex) Annual Mammography (beginning at age 40 or 50) Colon Cancer Screening (with flex sig.
Selecting the appropriate period between gos to is not extremely scientific. As such, you will see wide variation amongst practitioners, differing with accuity of illness, intricacy of care, and experience of the clinician. Perhaps more crucial is recognizing the proper situations for initiating contact along with the favored ways of communication (e.g., telephone, email, snail mail, and so on).
Not known Facts About Clinic - Dictionary Definition : Vocabulary.com
The system described above represents one particular organizational technique to outpatient care. There is a lot of room for variability. 09/18/98 Very first check out to me for this 56 yo male, previously cared for by Dr. M. He is to get all healthcare from me, and sees no other/outside service providers.
In fact taking: Glyburide 5 tid; Aspirin 325 qd; Fosinopril 20 qd; Diltiazem 60 tid. Allergic Reactions: None Active Issues/Events: DM: Understood x 2y with poor control over that time (alcs around 10). Client confused about medications. Claims has satisfied nutritional expert, however no education classes. No hypogly occasions. Has glucometer, but does not examine finger sticks.
Not like past mI. Not related to activity. Can occur up to 3x/w. Then might not take place for weeks. In some cases takes TNG for this, othertime not. No boost in frequency. S/P PTCA (? which vessel) in 93 at Sharp. Presented at that time with brand-new beginning of severe cp, diaphoresis, sob.
About What Is The Difference Between Hospital Nursing Vs Clinic ...
Uncertain if his MI was at this time or prior (though no comparable sx prior). No episodes/sx CHF. Last ETT-Thal at VA 95 ... 8 mets, fixed inf-septal flaw; little distal inf-septal area reperfusion (5% of myocardium). ER See: Went to the emergency situation space about 1 month back after having actually fallen approximately 5 feet from a ladder, landing on right ankle, with substantial associated pain.
Pain http://simonmgbe495.trexgame.net/facts-about-uc-san-diego-s-practical-guide-to-clinical-medicine-meded-uncovered in ankle now completlly solved. PMH: Diabetes (details as above) CAD (information as above) HTNHyperlipidemia PSH: S/P Appendectomy 88 Cigarette Smoking: ETOH: Other compound usage: 30 pack year, quit ten years ago. 2 beers per weekNone SOC: Not working presently, though wishes to go back to work doing light construction. what is a cheer clinic. Delights in reading and hiking.
Two children, ages 10 & 5, both well. Sexually active with partner, no issues with libido or erections. Family: Daddy died from MI, age 50; mother alive, age 65, though Hx DM (beginning 50), stroke age 60. One sibling, 2 sis all well. No household Hx cancer. PE: Obese male, NAD154/81 76 wt 208HEENT: NormalLungs: CTAC/V: s1 S2 no S3 S4 1/6 sem c/w aortic sclerosisABD: Soft, nt, no massesRectal: Brown stool, g neg; prostate nt, no nodulesGU: Testes descended bilat, nt, no masses; no herniaExt: no c/c/e Labs and Studies of Note: 09/98: T Chol 344, TG 651, HDL 48 (NOT FASTING), Cr 1, Glu 268, LFTS nl; UA + Protein, Alc 9.8 1/98: A1c 10, Glu 300 R Ankle Xray 8/98: neg ASSESSMENT/PLAN: 1.
Clinic - Description, Types, & Function - Britannica - Questions
Not actually taking Go here metformin and on incorrect dosing routine for glyb. Ned to readdress all areas of care. what is a women's health clinic. P: Will set up DM teaching Glyburid 10 quote No metformin for now (he's not taking it in any case). Evaluate action to glyburide and then add back ... will also enable simpler routines, at least at first.
attending to better control as above Had eye examination 6m earlier. 2. CAD/Chest Discomfort: Not sure what these 1-2 2nd episodes of chest pain are. They do not sound anginal. Not a worrisome pattern, offered reality that no boost in frequency, not with activity. However, client is not the very best historian and definitely does have CAD.P: Will organize for ETT-Thal to much better measure ex tol, examine for worrisome ischemiaD/C Diltiazem Start atenolol 25 Cont asa Offered bottle for fresh TNG s1, in case ...
HTN: Suboptimal controlP: D/C Diltiazem Fosinopril and atenolol as above 4. Hyperchol: Can't translate lipids in setting non-fasting state. P: Repeat profile on 12 hour fast D/C gemfibrozil (he is not taking it anyway) Would gain from statin if LDL > 100 ... likewise would definitely gain from much better glycemic control ... to be attended to as above.
Some Known Incorrect Statements About Clinic Vs. Hospital - Blog - Amopportunities
That provides a distinction for traditional medical care clinics. According to MGMA information, the typical overall number of encounters in household medication centers without obstetrics services reduced 9.9 percent in between 2015 and 2018. The typical relative value units (RVUs), though, decreased just 0.3 percent. Those numbers show that while physicians are seeing fewer clients, they're seeing more complex clients and cases."I believe a lot of people want a relationship with a doctor who will truly manage their care carefully," Hajde states.
Increased gain access to points for customers can be a good thing, particularly in backwoods where there is a lack of medical care suppliers, states Gary LeRoy, MD, a family doctor in Dayton, Ohio and president of that American Academy of Household Physicians (AAFP)."The supreme goal would be to supply comprehensive longitudinal coordinated care for patients from coast to coast, east to west, north to south.
And these retail health-type centers can often provide the needed immunizations and health care information that underserved areas are in desperate need of."This increased access can cause fragmented care, however, due to the fact that retail clinics do not have a system for sharing records and patients do not always remember what happened throughout a check out or assessment."If you get a vaccine at a CVS or some other freestanding center, and you do not offer a copy of the documents they provide to you to your medical care physician, it can develop a gap in care," Hadje states.
You ask someone what medications they're on, they do not know. They state they take one blue tablet, one red pill, one white pill."Probably one of the important things that frustrates doctors more than anything else is when they need to see patients and they do not have a complete copy of their medical record for all the facilities they have actually been to.
She was initially told it was allergic reactions, then bronchitis. They put her on multiple medications. However Abraham detected a knew from her records that the client had had breast cancer more than 20 years previous and diagnosed her with a lung embolism. If she 'd concern Abraham sooner, the embolism might have been found earlier.
Instead they go to the professional and the PCP falls out of the loop of care."We do not wish to develop a situation like with relay races, where people lose due to the fact that they drop the baton handoff," LeRoy says. "That's essentially what's taking place here. You put more runners in the race, there are more opportunities to hand off the baton-and more opportunities to drop the baton since they're not efficiently practiced in handoffs."Health care customers have ended up being utilized to getting the products and services they desire where and when they want them; they anticipate the very same from their healthcare suppliers."Health care delivery in traditional centers truly is going to need to progress to be quicker, much better, less expensive and quicker in order for people to be pleased with it.
Main care doctors require to listen to their clients and look at ways to meet consumers' requirements within conventional practices, states Michael Munger, MD, with St. Luke's Health System in Kansas City."The onus is on main care doctors to deliver what our clients require," he states. "How can I make certain I'm offered to patients? In some cases that could be as simple as ensuring you have somebody on call for your practice 24 hr a day, 7 days a week.
The Ultimate Guide To How Much Is An Iud At Unc Health Clinic
Maybe you'll just inform them they need to be seen in urgent care, but if they've interacted with you before they go, you know that you have something to follow up with. You understand you need to close the loop."Main care centers need to create methods for patients with intense diseases to be seen that same day.

Munger keeps in mind that numerous family doctor nationwide have actually already set up some kind of sophisticated access, extended hours or ability for walk-in and same-day availability. Strong relationships with patients and exceptional total patient service can form the bonds that bring them back to your practice for all their requirements. That implies making sure your center is contending on a technological level.
"Those are all things that if they can't meet that requirement, it's going to be actually difficult for conventional clinics to contend with these retail and immediate care centers."LeRoy and Munger say developing relationships with local urgent care and retail clinics can be useful for conventional healthcare clinics, too."If I'm a family physician and I have an independent practice, I would be connecting to the retail clinics around me and making certain I let them understand I'm here if my patient shows up," Munger states.
They can be part of that neighborhood, however we have to talk with each other."Greater collaboration between service providers would assist attend to the fragmented care. But the universal technology isn't there yet. So the burden for quality, constant care likewise falls to patients."Pushing customers to become more responsible for their own individual health and care will be substantial moving into the future," Hajde states.
To assist that occur, medical care doctors need to speak with their clients about when to check out a retail or urgent care clinic, and they need to emphasize the value of precisely and fully interacting what occurred throughout those visits to their main care doctor."That's the very best method to guarantee care is collaborated," he says - what is average marketing cost for mobile health clinic.
"But it's a two-way street. [Retail clinics] require to comprehend what we do and comprehending that even if it is called primary care, doesn't imply that it's simple care, since there's absolutely nothing easy about what we do.".
With the boom of on-demand healthcare, lots of kinds of instant care are now offered to patients. However, the client can be puzzled by which place of treatment they must seek. And it's not unexpected, given the similar-sounding names for differing care. How do you help clients comprehend the distinction in between walk-in retail clinics and urgent care centers? To help patients choose the appropriate care, it's your task as an immediate care center to educate patients about the distinctions between your urgent care and the alternatives.
How What Is A Health Care Clinic can Save You Time, Stress, and Money.
Think about adding a services checklist that distinguishes between what your center uses vs. others for quick contrast. Here's a fast summary you can show patients about the differences in between walk-in retail and immediate care centers. "Walk-in" is a little a misleading term. Both retail and immediate cares are "walk-in" or "no appointment required".
Retail centers fill the need for quick, less complicated health needs that can be served outside the medical professional's office or urgent care. Solutions include treatment of uncomplicated illness, such as a sore throat or earache, or preventative care like vaccines or physical examinations. In addition, retail clinics are usually a clinic-within-a-store model with minimal area, and are staffed by nurse practitioners or physician assistants. She was emphatic about having a physician who knew her name and cared to ask her opinion. Millie was not ready to get an influenza chance at a retail clinic, so there is no doubt she would not look for care at one when she was ill. In truth, I visited her house to give her the influenza vaccine myself for many years.
It is throughout one of those house gos to when I initially found out Millie had lost her father to influenza during the epidemic of 1918. It seems perverse to deliver health care services at a location called the MinuteClinic. The sort of physician-patient relationship that can be cultivated in a minute is not one to compose house about. what is the spectrum health neurology headache clinic.
Seamless environments are no match for a "determination to put professional expertise at the feet of childhood magic." The bond Millie and I shared was magical. And every client should have a doctor who knows their name. Niran S. Al-Agba is a pediatrician and can be reached at her self-titled website, Dr.
An outpatient center located in a grocery, drug shop, retail shop, or supermarket. It provides a concentrated series of protocol-driven health care services, such as the treatment of minor health problems or injuries, and the administration of vaccinations.
Insights by: Dennie KimWritten by: Andrew Offer In a current White Home instruction, numerous corporate leaders existed as the president declared a national emergency situation. You may not have acknowledged some of them, but they were leaders of several large corporations (e.g. Target, CVS, Walgreens, Walmart) that are coordinating with federal government companies in an effort to "flatten the curve" of COVID-19.
The actions they take as essential gamers in health care delivery will have a considerable influence on public security, and their quick actions intend to prevent the disease from frustrating our health care system. Even 10 years ago, we would not be talking about retail health centers having such a crucial function in public safety.
The Buzz on How Is A Clinic Different Than A Primary Health Care Provided
It is not simply their unusual area that makes them different from other clinics and physician's offices at a retail center, you probably won't see a doctor at all! Instead, clients of a retail clinic will more than likely be dealt with by a nurse professional or doctor assistant. This kind of health care shipment just came onto the scene in 2000 in Minnesota as a pilot called "QuickMedx." Really rapidly this innovative new kind of health care shipment, featuring a nontraditional physical space and nontraditional physician, took hold across the country.
Filling a Gap, Establishing TrustIn the past years, retail centers have ended up being even more extensive, in addition to more accepted by people as a legitimate location to go see a doctor. This kind of healthcare filled a need in the market for practical, prompt and premium medical care treatment, attending https://transformationstreatment1.blogspot.com/2020/07/common-co-occurring-disorders.html to enduring problems of access to fundamental health care services in numerous neighborhoods.
Now, this success puts them on the frontlines of challenging a pandemic that is evaluating the limitations of our present healthcare infrastructure. "The U.S. reaction to COVID-19 shines a brilliant light on issues of gain access to and capability in the existing healthcare delivery facilities an inefficiency that retail centers have actually been attempting to resolve given that their creation in 2000," says Professor Dennie Kim, who specializes in healthcare shipment and reform and has actually been studying the spread of retail centers in partnership with Professors Roman Galperin at the Johns Hopkins Carey School of Service and Gurneeta Vasudeva Singh at the University of Minnesota's Carlson School of Management.
We see that these centers are presently playing an essential function in the reaction, assisting reduce the load on medical facilities by offering basic health care services in stores where individuals are going shopping for necessities and keeping people house through telemedicine." Swiftly Sharing Duty for Public SafetyWith over 3,000 areas, the national circulation of retail health clinics enables for massive coordination throughout states in an effort to safeguard the communities they serve from the COVID-19 hazard.
For instance, CVS Health and MinuteClinic have taken numerous measures to protect its stakeholders throughout the COVID-19 break out including: Supplying perks and other benefits to numerous existing retail employees, as well as working with thousands of brand-new full-time and part-time personnel to deal with an increased demand for health care services. All consultations are to be set up online to prevent infections from unscheduled walk-in check outs among patients - how to collect demographic data for health clinic.
They may receive assistance to instead go to a different healthcare setting that much better satisfies their requirements offered the patient's specific situations. Video gos to are being interacted as the most safe method for patients to interact with doctor when possible. Retail Clinics in the Days AheadThe existing scenario might make clients, and healthcare professionals, a lot more comfy with these more novel approaches of receiving health care services.
" Anything that enables clients to seek medical advice while lowering volume at medical facilities and decreasing unneeded direct exposure and spread will add to 'flattening the curve.'" With their strong value proposal, retail centers quickly filled a need in our healthcare system for a narrow set of services. Existing events demonstrate that they are now an integral player in dealing with a pandemic that threatens neighborhood health and there is evidence that retail business have an interest in expanding their healthcare offerings (e.g., Walmart University Hospital, CVS Health).
What Time Does Jps Behavioral Health Clinic Care Open Things To Know Before You Get This
Hunter, Lauren P. PhD, CNM, WHCNP1, a; Weber, Charles E. PharmD (Consultant) 2, b; Morreale, Anthony P. PharmD, MBA3; Wall, James H. CPhT4, c aAssociate Professor and Nurse-Midwife Program Director bDirector, Financier Relations cPharmacy Technician and Undergrad Student 1San Diego State University, College of Health and Human Being Providers, School of Nursing, San Diego, California 2Pacific Enterprises, La Jolla, California 3MediMin Inc., La Jolla, California 4University of the Pacific, Stockton, California Lauren P.

Tel: 858-454-9033; E-mail: Gotten: July 2008; accepted: September 2008 Dr. Hunter, Dr. Morreale and Dr. Weber all own stock in MediMin. Dr. Morreale is the Diretor of Financier relations for MediMin. doi: 10.1111/ j. 1745-7599.2009.00447. x.
June 28, 2018 - Retail centers are gaining in popularity amongst patients looking for fast, practical care for minor conditions. Kiosks and no-appointment-needed workplaces located in corner pharmacies and huge box stores have the prospective to keep clients out of pricey emergency spaces or hectic primary care providers. Yet concerns about overutilization for concerns that might not need any treatment at all can hold payers back from offering repayment for these services.
Currently there are over 2000 retail clinics across the United States. This number is expected to grow as drug store chains and other sellers start to see returns from their investments in these clinics. Retails clinics are often confused with immediate care centers, however the 2 kinds of organizations provide different services.
Retail centers generally employ qualified nurse practitioners (NPs) and/or physician assistants (PAs) to administer treatment. Self-reliance Blue Cross discusses that retail centers can be helpful for beneficiaries seeking remedy for cuts and external injuries, cough or https://transformationstreatment1.blogspot.com/2020/07/anxiety-disorders-treatment.html sore throat, ear and sinus discomfort, small fevers, or rashes. An urgent care center is a medical facility that usually employs doctor assistants and nurse professionals that are supervised by board-certified physicians.
Clinic Vs Hospital: How To Choose The Best Working ... Things To Know Before You Buy
That uses a differentiation for traditional medical care clinics. According to MGMA data, the typical overall number of encounters in household medication clinics without obstetrics services decreased 9.9 percent between 2015 and 2018. The average relative worth systems (RVUs), though, reduced just 0.3 percent. Those numbers indicate that while doctors are seeing less clients, they're seeing more intricate clients and cases."I believe many people desire a relationship with a doctor who will truly handle their care carefully," Hajde states.
Increased gain access to points for customers can be an advantage, especially in rural areas where there is a shortage of medical care service providers, says Gary LeRoy, MD, a household doctor in Dayton, Ohio and president of that American Academy of Family Physicians (AAFP)."The supreme objective would be to offer extensive longitudinal coordinated care for clients from coast to coast, east to west, north to south.

And these retail health-type centers can in some cases supply the needed immunizations and health care information that underserved locations are in desperate requirement of."This increased gain access to can cause fragmented care, though, because retail centers do not have a system for sharing records and clients don't constantly remember what occurred during a go to or consultation."If you get a vaccine at a CVS or some other freestanding facility, and you do not offer a copy of the documents they provide to you to your main care doctor, it can produce a gap in care," Hadje says.
You ask someone what medications they're on, they do not know. They state they take one blue pill, one red pill, one white pill."Most likely among the things that frustrates doctors more than anything else is when they need to see patients and they don't have a total copy of their medical record for all the centers they have actually been to.
She was at first informed it was allergies, then bronchitis. They put her on multiple medications. However Abraham detected a knew from her records that the patient had had breast cancer more than 20 years previous and diagnosed her with a lung embolism. If she 'd concern Abraham earlier, the embolism might have been discovered previously.
Rather they go to the professional and the PCP falls out of the loop of care."We don't want to create a circumstance like with relay races, where individuals lose due to the fact that they drop the baton handoff," LeRoy states. "That's essentially what's happening here. You put more runners in the race, there are more chances to hand off the baton-and more chances to drop the baton because they're not efficiently practiced in handoffs."Health care customers have actually ended up being utilized to getting the product or services they want where and when they want them; they expect the very same from their doctor."Healthcare delivery in traditional centers really is going to need to develop to be quicker, better, more affordable and much faster in order for individuals to be satisfied with it.
Main care doctors require to listen to their patients and take a look at methods to meet customers' needs within traditional practices, states Michael Munger, MD, with St. Luke's Health System in Kansas City."The onus is on medical care physicians to provide what our patients require," he says. "How can I make sure I'm offered to clients? Sometimes that could be as straightforward as ensuring you have someone on call for your practice 24 hr a day, seven days a week.
How Much Is An Iud At Unc Health Clinic for Dummies
Maybe you'll just tell them they need to be seen in immediate care, however if they've interacted with you prior to they go, you understand that you have something to follow up with. You know you need to close the loop."Medical care clinics require to produce ways for clients with acute health problems to be seen that same day.
Munger notes that numerous family physicians nationwide have currently set up some type of sophisticated access, extended hours or capability for walk-in and same-day schedule. Strong relationships with patients and extraordinary total patient service can form the bonds that bring them back to your practice for all their requirements. That implies making sure your clinic is completing on a technological level.
"Those are all things that if they can't meet that need, it's going to be actually hard for conventional centers to contend with these retail and urgent care clinics."LeRoy and Munger say developing relationships with regional immediate care and retail clinics can be useful for traditional health care centers, too."If I'm a family doctor and I have an independent practice, I would be reaching out to the retail clinics around me and making sure I let them understand I'm here if my client appears," Munger states.
They can be part of that neighborhood, however we need to talk with each other."Greater partnership between companies would help attend to the fragmented care. However the universal technology isn't there yet. So the concern for quality, continuous care also is up to clients."Pushing consumers to end up being more accountable for their own individual health and care will be substantial moving into the future," Hajde says.
To help that occur, medical care physicians must talk with their clients about when to check out a retail or immediate care clinic, and they must highlight the value of properly and completely interacting what occurred throughout those check outs to their primary care physician."That's the best method to make sure care is coordinated," he states - what is retail health clinic.
"But it's a two-way street. [Retail clinics] need to understand what we do and understanding that even if it is called medical care, does not indicate that it's simple care, because there's absolutely nothing easy about what we do.".
With the boom of on-demand health care, many kinds of immediate care are now available to patients. Nevertheless, the patient can be confused by which place of treatment they should seek. And it's not unexpected, offered the similar-sounding names for differing care. How do you assist clients comprehend the difference in between walk-in retail clinics and immediate care centers? To help patients pick the proper care, it's your task as an immediate care center to inform patients about the distinctions between your immediate care and the options.
All about What Health Insurance Does The Cleveland Clinic Accept?
Consider including a services checklist that compares what your clinic uses vs. others for quick comparison. Here's a quick introduction you can share with clients about the distinctions in between walk-in retail and immediate care centers. "Walk-in" is a little bit of a misleading term. Both retail and immediate cares are "walk-in" or "no consultation required".
Retail clinics fill the requirement for fast, less intricate health requires that can be served outside the medical professional's office or urgent care. Services consist of treatment of uncomplicated disease, such as a sore throat or earache, or preventative care like vaccines or physical exams. In addition, retail centers are typically a clinic-within-a-store design with restricted area, and are staffed by nurse professionals or doctor assistants. She was emphatic about having a physician who understood her name and cared to ask her viewpoint. Millie was not prepared to get an influenza shot at a retail clinic, so there is no doubt she would not seek care at one when she was ill. In reality, I visited her home to offer her the influenza vaccine myself throughout the years.
It is throughout among those home check outs when I first found out Millie had lost her daddy to influenza during the epidemic of 1918. It seems perverse to deliver healthcare services at a location called the MinuteClinic. The kind of physician-patient relationship that can be cultivated in a minute is not one to write home about. what are the hours for millennium physicians clinic on 1735 sw health center naples florida.
Seamless environments are no match for a "desire to put professional know-how at the feet of childhood magic." The bond Millie and I shared was magical. And every client should have a physician who understands their name. Niran S. Al-Agba is a pediatrician and can be reached at her self-titled website, Dr.
An outpatient clinic located in a grocery, drug shop, store, or grocery store. It provides a focused range of protocol-driven healthcare services, such as the treatment of small illnesses or injuries, and the administration of vaccinations.
Insights by: Dennie KimWritten by: Andrew Sell In a recent White Home rundown, numerous corporate leaders existed as the president declared a nationwide emergency. You may not have acknowledged some of them, but they were leaders of a number of big corporations (e.g. Target, CVS, Walgreens, Walmart) that are coordinating with federal government companies in an effort to "flatten the curve" of COVID-19.

The actions they take as key players in health care shipment will have a considerable influence on public safety, and their swift actions intend to prevent the illness from overwhelming our healthcare system. Even ten years back, we would not be talking about retail health clinics having such an essential function in public security.
The 15-Second Trick For What Is The Address For Jps Health Clinic Viola Pitts
It is not just their unusual location that makes them different from other clinics and physician's offices at a retail center, you most likely won't see a medical professional at all! Rather, clients of a retail center will more than likely be dealt with by a nurse professional or doctor assistant. This form of health care delivery just came onto the scene in 2000 in Minnesota as a pilot called "QuickMedx." Very quickly this innovative new type of health care delivery, featuring a nontraditional physical space and nontraditional physician, took hold nationwide.
Filling a Space, Establishing TrustIn the previous decade, retail centers have become a lot more prevalent, along with more accepted by people as a genuine location to go see a medical specialist. This form of healthcare filled a requirement in the market for practical, timely and top quality medical care treatment, resolving long-lasting issues of access to standard health care services in lots of communities.
Now, this success puts them on the frontlines of facing a pandemic that is checking the limitations of our current health care facilities. "The U.S. action to COVID-19 shines an intense light on problems of gain access to and capability in the existing healthcare delivery infrastructure an inefficiency that retail centers have actually been attempting to address since their creation in 2000," states Teacher Dennie Kim, who concentrates on healthcare shipment and reform and has actually been studying the spread of retail centers in collaboration with Professors Roman Galperin at the Johns Hopkins Carey School of Organization and Gurneeta Vasudeva Singh at the University of Minnesota's Carlson School of Management.
We see that these centers are currently playing a crucial function in the reaction, helping in reducing the load on health centers by offering basic healthcare services in stores where individuals are purchasing requirements and keeping individuals house through telemedicine." Swiftly Sharing Obligation for Public SafetyWith over 3,000 locations, the nationwide circulation of retail health centers enables large-scale coordination throughout states in an effort to safeguard the neighborhoods they serve from the COVID-19 threat.
For instance, CVS Health and MinuteClinic have taken a number of procedures to protect its stakeholders throughout the COVID-19 break out including: Offering bonus offers and other advantages to numerous existing retail staff members, as well as working with countless new full-time and part-time staff to handle an increased demand for healthcare services. All visits are to be arranged online to prevent infections from unscheduled walk-in visits among patients - how does health insurance work at a clinic.
They might receive guidance to rather visit a different healthcare setting that better meets their requirements offered the client's specific scenarios. Video check outs are being communicated as the safest method for clients to engage with doctor when possible. Retail Clinics in the Days AheadThe present circumstance might make clients, and healthcare specialists, a lot more comfortable with these more unique techniques of receiving healthcare services.
" Anything that makes it possible for clients to look for medical suggestions while minimizing volume at medical facilities and decreasing unnecessary direct exposure and spread will contribute to 'flattening the curve.'" With their strong value proposal, retail clinics rapidly filled a need in our healthcare system for a narrow set of services. Current events show that they are now an essential gamer in taking on a pandemic that threatens neighborhood health and there is proof that retail companies are interested in broadening their health care offerings (e.g., Walmart University Hospital, CVS Health).
Some Ideas on How Is A Clinic Different Than A Primary Health Care Provided You Need To Know
Hunter, Lauren P. PhD, CNM, WHCNP1, a; Weber, Charles E. PharmD (Expert) 2, b; Morreale, Anthony P. PharmD, MBA3; Wall, James H. CPhT4, c aAssociate Professor and Nurse-Midwife Program Director bDirector, Financier Relations cPharmacy Service technician and Undergraduate Trainee 1San Diego State University, College of Health and Human Solutions, School of Nursing, San Diego, California 2Pacific Enterprises, La Jolla, California 3MediMin Inc., La Jolla, California 4University of the Pacific, Stockton, California Lauren P.
Tel: 858-454-9033; E-mail: Gotten: July 2008; accepted: September 2008 Dr. Hunter, Dr. Morreale and Dr. Weber all own stock in MediMin. Dr. Morreale is the Diretor of Financier relations for MediMin. doi: 10.1111/ j. 1745-7599.2009.00447. x.
June 28, 2018 - Retail clinics are gaining in popularity amongst clients looking for quick, convenient look after minor ailments. Kiosks and no-appointment-needed offices located in corner drug stores and big box stores have the potential to keep clients out of expensive emergency rooms or hectic medical care providers. Yet concerns about overutilization for concerns that may not need any treatment at all can hold payers back from providing compensation for these services.
Presently there are over 2000 retail clinics across the United States. This number is anticipated https://transformationstreatment1.blogspot.com/2020/07/anxiety-disorders-treatment.html to grow as pharmacy chains and other merchants start to see returns from their financial investments in these clinics. Retails clinics are sometimes confused with immediate care centers, however the two kinds of organizations offer various services.
Retail centers typically utilize licensed nurse practitioners (NPs) and/or doctor assistants (PAs) to administer treatment. Self-reliance Blue Cross explains that retail centers can be handy for recipients seeking relief from cuts and external injuries, cough or aching throat, ear and sinus pain, small https://transformationstreatment1.blogspot.com/2020/07/common-co-occurring-disorders.html fevers, or rashes. An immediate care center is a medical center that usually uses physician assistants and nurse practitioners that are supervised by board-certified doctors.
What's The Difference Between A Hospital And A Clinic? - Quora for Dummies
That uses a distinction for standard medical care centers. According to MGMA data, the mean overall number of encounters in family medication centers without obstetrics services reduced 9.9 percent in between 2015 and 2018. The mean relative worth systems (RVUs), however, decreased simply 0.3 percent. Those numbers suggest that while physicians are seeing less clients, they're seeing more intricate clients and cases."I think the majority of individuals desire a relationship with a doctor who will really handle their care closely," Hajde says.
Increased gain access to points for customers can be a good idea, particularly in backwoods where there is a lack of medical care service providers, says Gary LeRoy, MD, a household doctor in Dayton, Ohio and president of that American Academy of Family Physicians (AAFP)."The supreme goal would be to offer comprehensive longitudinal coordinated care for patients from coast to coast, east to west, north to south.
And these retail health-type centers can in some cases provide the required immunizations and healthcare information that underserved locations remain in desperate requirement of."This increased gain access to can trigger fragmented care, though, since retail centers do not have a system for sharing records and patients don't constantly remember what took location during a see or consultation."If you get a vaccine at a CVS or some other freestanding center, and you don't supply a copy of the documents they provide to you to your main care physician, it can create a space in care," Hadje states.
You ask someone what medications they're on, they do not understand. They state they take one blue pill, one red tablet, one white pill."Probably one of the things that frustrates physicians more than anything else is when they have to see patients and they do not have a complete copy of their medical record for all the centers they have actually been to.
She was at first informed it was allergies, then bronchitis. They put her on multiple medications. But Abraham detected a knew from her records that the patient had actually had breast cancer more than twenty years previous and diagnosed her with a lung embolism. If she 'd concern Abraham sooner, the embolism might have been found previously.
Rather they go to the professional and the PCP falls out of the loop of care."We don't want to create a scenario like with relay races, where individuals lose since they drop the baton handoff," LeRoy states. "That's generally what's occurring here. You put more runners in the race, there are more chances to hand off the baton-and more opportunities to drop the baton since they're not successfully practiced in handoffs."Health care consumers have become utilized to getting the product or services they desire where and when they want them; they expect the exact same from their doctor."Healthcare delivery in conventional centers really is going to have to evolve to be quicker, better, less expensive and quicker in order for individuals to be satisfied with it.
Medical care physicians require to listen to their clients and look at methods to fulfill consumers' requirements within standard practices, says Michael Munger, MD, with St. Luke's Health System in Kansas City."The onus is on primary care physicians to provide what our patients need," he says. "How can I make certain I'm available to clients? Often that might be as uncomplicated as ensuring you have someone on call for your practice 24 hours a day, 7 days a week.
The 30-Second Trick For What Time Does Jps Behavioral Health Clinic Care Open
Perhaps you'll simply inform them they require to be seen in urgent care, but if they've communicated with you before they go, you understand that you have something to follow up with. You know you need to close the loop."Medical care clinics need to create methods for patients with acute diseases to be seen that very same day.
Munger notes that many family doctor nationwide have actually currently instituted some kind of advanced access, extended hours or ability for walk-in and same-day availability. Strong relationships with clients and exceptional total client service can form the bonds that bring them back to your practice for all their needs. That implies ensuring your clinic is contending on a technological level.
"Those are all things that if they can't meet that requirement, it's going to be really challenging for standard centers to take on these retail and immediate care centers."LeRoy and Munger state establishing relationships with local immediate care and retail clinics can be useful for conventional health care centers, too."If I'm a family doctor and I have an independent practice, I would be connecting to the retail clinics around me and ensuring I let them know I'm here if my patient shows up," Munger states.
They can be part of that neighborhood, however we need to talk with each other."Greater cooperation in between suppliers would help attend to the fragmented care. However the universal innovation isn't there yet. So the problem for quality, continuous care likewise is up to clients."Pushing customers to become more accountable for their own individual health and care will be substantial moving into the future," Hajde states.
To assist that take place, main care doctors need to talk with their patients about when to go to a retail or urgent care clinic, and they must stress the value of properly and totally interacting what took place throughout those sees to their medical care doctor."That's the best way to guarantee care is collaborated," he states - what is the square footage required for a health clinic.
"But it's a two-way street. [Retail clinics] need to understand what we do and comprehending that even if it is called medical care, does not mean that it's simple care, due to the fact that there's nothing simple about what we do.".
With the boom of on-demand healthcare, numerous kinds of instant care are now offered to clients. Nevertheless, the client can be confused by which location of treatment they need to look for. And it's not unexpected, provided the similar-sounding names for varying care. How do you help clients understand the difference between walk-in retail centers and immediate care centers? To help clients choose the proper care, it's your job as an urgent care center to educate clients about the differences between your urgent care and the options.
The 8-Second Trick For What Is The Address For Jps Health Clinic Viola Pitts
Consider including a services checklist that compares what your center provides vs. others for fast comparison. Here's a quick overview you can show clients about the distinctions between walk-in retail and urgent care clinics. "Walk-in" is a little a misleading term. Both retail and immediate cares are "walk-in" or "no visit required".
Retail centers fill the requirement for quick, less complex health needs that can be served outside the physician's workplace or urgent care. Solutions consist of treatment of straightforward illness, such as an aching throat or earache, or preventative care like vaccines or physical examinations. In addition, retail centers are generally a clinic-within-a-store design with limited space, and are staffed by nurse professionals or physician https://transformationstreatment1.blogspot.com/2020/07/common-co-occurring-disorders.html assistants. She was emphatic about having a physician who knew her name and cared to ask her viewpoint. Millie was not prepared to get a flu shot at a retail center, so there is no doubt she would not look for care at one when she was ill. In fact, I visited her home to give her the influenza vaccine myself over the years.
It is throughout one of those home gos to when I initially found out Millie had actually lost her daddy to influenza during the epidemic of 1918. It appears perverse to provide health care services at a location called the MinuteClinic. The sort of physician-patient relationship that can be cultivated in a minute is not one to compose house about. what do you need to own a mental health clinic.
Seamless communities are no match for a "desire to put professional expertise at the feet of youth magic." The bond Millie and I shared was wonderful. And every patient should have a doctor who understands their name. Niran S. Al-Agba is a pediatrician and can be reached at her self-titled website, Dr.
An outpatient center situated in a grocery, drug store, retail store, or grocery store. It offers a focused variety of protocol-driven health care https://transformationstreatment1.blogspot.com/2020/07/anxiety-disorders-treatment.html services, such as the treatment of minor illnesses or injuries, and the administration of vaccinations.
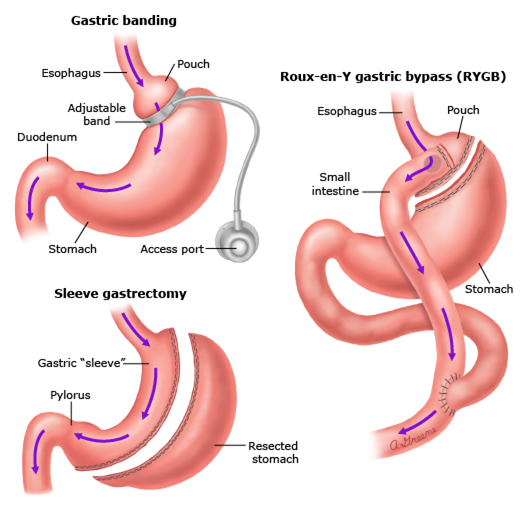
Insights by: Dennie KimWritten by: Andrew Sell In a recent White House briefing, a number of corporate leaders existed as the president stated a national emergency. You might not have recognized a few of them, but they were leaders of a number of large corporations (e.g. Target, CVS, Walgreens, Walmart) that are collaborating with government companies in an effort to "flatten the curve" of COVID-19.
The actions they take as crucial gamers in health care delivery will have a considerable influence on public safety, and their swift actions intend to avoid the illness from overwhelming our healthcare system. Even ten years earlier, we would not be speaking about retail health clinics having such an essential function in public safety.
How How To Open A Health Clinic can Save You Time, Stress, and Money.
It is not simply their unusual area that makes them different from other centers and medical professional's offices at a retail center, you most likely won't see a physician at all! Rather, patients of a retail clinic will more than likely be dealt with by a nurse professional or physician assistant. This type of health care shipment just came onto the scene in 2000 in Minnesota as a pilot called "QuickMedx." Very quickly this innovative new type of health care shipment, including a nontraditional physical area and nontraditional doctor, took hold across the country.
Filling a Gap, Developing TrustIn the previous decade, retail centers have actually ended up being much more extensive, as well as more accepted by people as a legitimate location to go see a doctor. This kind of healthcare filled a requirement in the market for convenient, timely and high-quality medical care treatment, resolving long-lasting issues of access to fundamental health care services in lots of neighborhoods.
Now, this success puts them on the frontlines of challenging a pandemic that is testing the limitations of our current health care infrastructure. "The U.S. action to COVID-19 shines an intense light on problems of gain access to and capability in the existing health care shipment infrastructure an inadequacy that retail centers have been trying to address since their inception in 2000," states Teacher Dennie Kim, who concentrates on healthcare delivery and reform and has actually been studying the spread of retail centers in partnership with Professors Roman Galperin at the Johns Hopkins Carey School of Company and Gurneeta Vasudeva Singh at the University of Minnesota's Carlson School of Management.
We see that these centers are presently playing a crucial function in the response, helping in reducing the load on healthcare facilities by supplying basic healthcare services in stores where people are buying needs and keeping individuals home through telemedicine." Promptly Sharing Responsibility for Public SafetyWith over 3,000 locations, the national circulation of retail health clinics enables massive coordination across states in an effort to safeguard the neighborhoods they serve from the COVID-19 threat.
For example, CVS Health and MinuteClinic have taken numerous measures to safeguard its stakeholders throughout the COVID-19 break out including: Offering perks and other advantages to many current retail workers, along with hiring thousands of brand-new full-time and part-time staff to manage an increased need for healthcare services. All appointments are to be arranged online to prevent infections from unscheduled walk-in visits amongst patients - what is average marketing cost for mobile health clinic.
They might receive guidance to rather check out a various health care setting that much better fulfills their requirements given the client's particular situations. Video check outs are being interacted as the safest method for clients to communicate with physician when possible. Retail Clinics in the Days AheadThe current scenario might make patients, and healthcare professionals, a lot more comfortable with these more novel approaches of getting healthcare services.
" Anything that enables patients to seek medical advice while minimizing volume at healthcare facilities and lessening unnecessary exposure and spread will add to 'flattening the curve.'" With their strong value proposal, retail clinics quickly filled a need in our health care system for a narrow set of services. Current occasions show that they are now an essential gamer in tackling a pandemic that threatens community health and there is evidence that retail companies are interested in expanding their health care offerings (e.g., Walmart University Hospital, CVS Health).
7 Easy Facts About How To Start Rural Health Clinic Book Described
Hunter, Lauren P. PhD, CNM, WHCNP1, a; Weber, Charles E. PharmD (Expert) 2, b; Morreale, Anthony P. PharmD, MBA3; Wall, James H. CPhT4, c aAssociate Teacher and Nurse-Midwife Program Director bDirector, Financier Relations cPharmacy Specialist and Undergraduate Trainee 1San Diego State University, College of Health and Human Providers, School of Nursing, San Diego, California 2Pacific Enterprises, La Jolla, California 3MediMin Inc., La Jolla, California 4University of the Pacific, Stockton, California Lauren P.
Tel: 858-454-9033; Email: Gotten: July 2008; accepted: September 2008 Dr. Hunter, Dr. Morreale and Dr. Weber all own stock in MediMin. Dr. Morreale is the Diretor of Financier relations for MediMin. doi: 10.1111/ j. 1745-7599.2009.00447. x.
June 28, 2018 - Retail centers are getting in appeal amongst patients searching for fast, hassle-free care for small conditions. Kiosks and no-appointment-needed workplaces located in corner pharmacies and huge box shops have the potential to keep clients out of costly emergency clinic or hectic medical care companies. Yet concerns about overutilization for concerns that may not require any treatment at all can hold payers back from offering repayment for these services.
Currently there are over 2000 retail clinics throughout the United States. This number is expected to grow as pharmacy chains and other merchants start to see returns from their financial investments in these centers. Retails clinics are in some cases confused with urgent care centers, however the two types of companies offer different services.
Retail centers generally employ qualified nurse practitioners (NPs) and/or physician assistants (PAs) to administer treatment. Independence Blue Cross explains that retail centers can be useful for beneficiaries seeking relief from cuts and external injuries, cough or aching throat, ear and sinus discomfort, minor fevers, or rashes. An immediate care center is a medical center that generally utilizes physician assistants and nurse specialists that are supervised by board-certified doctors.


